What is secondary prevention of obesity

Prevention Strategies & Guidelines
To reverse the obesity epidemic, places and practices need to support healthy eating and active living in many settings. Below are recommended strategies to prevent obesity.
Nutrition, Physical Activity, and Obesity Prevention Strategies
The CDC Guide to Strategies to Increase Physical Activity in the Community [PDF-1.2MB] provides guidance for program managers, policy makers, and others on how to select strategies to increase physical activity.
Physical Activity: Built Environment Approaches Combining Transportation System Interventions with Land Use and Environmental DesignThe Community Preventive Services Task Force recommends built environment strategies that combine one or more interventions to improve pedestrian or bicycle transportation systems with one or more land use and environmental design interventions to increase physical activity.
The CDC Guide to Strategies to Increase the Consumption of Fruits and Vegetables [PDF-2.1MB] provides guidance for program managers, policy makers, and others on how to select strategies to increase the consumption of fruits and vegetables.
The CDC Guide to Breastfeeding Interventions provides state and local community members information to choose the breastfeeding intervention strategy that best meets their needs.
Recommended Community Strategies and Measurements to Prevent Obesity in the United States [PDF-376KB] contains 24 recommended obesity prevention strategies focusing on environmental and policy level change initiatives that can be implemented by local governments and school districts to promote healthy eating and active living.
Early Care and Education Strategies
CDCs framework for obesity prevention, in the ECE setting is known as the Spectrum of Opportunities [PDF-666KB]. The Spectrum identifies ways that states, and to some extent communities, can support child care and early education facilities to achieve recommended standards and best practices for obesity prevention. The Spectrum aligns with comprehensive national ECE standards for obesity prevention address nutrition, infant feeding, physical activity and screen time, Caring for Our Children: National Health and Safety Performance Standards (CFOC), 3rd ed.
School Health Guidelines
School Health Guidelines to Promote Healthy Eating and Physical Activity provides nine guidelines that serve as the foundation for developing, implementing, and evaluating school-based healthy eating and physical activity policies and practices for students in grades K-12.
The following resources are designed to assist schools and program coordinators to inform stakeholders and school health services staff on obesity facts, engaging students and managing chronic health conditions.
Community Guide
The Community Guide Obesity Prevention and Control is a free resource to help you choose programs and policies to prevent and control obesity in your community.
Clinical Guidelines
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents [PDF-3.26MB] This resource summarizes the integrated guidelines develop by the Federal Government to address cardiovascular disease in children and adolescents.
Screening for Obesity in Pediatric Primary Care: Recommendations from the U.S. Preventive Services Task Force Guidance for primary care providers in screening for obesity and offering or referring to comprehensive, intensive behavioral weight management interventions.
The American Academy of Pediatrics Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents With Obesity aims to inform pediatricians and other pediatric health care providers about the standard of care for evaluating and treating children with overweight and obesity and related comorbidities. The CPG promotes an approach that considers the childs health status, family system, community context, and resources for treatment to create the best evidence-based treatment plan.
2013 Guideline on the Assessment of Cardiovascular RiskThis is a Report of the American College of Cardiology and the American Heart Association Task Force on Practice Guidelines for reducing the risk of cardiovascular disease.
School-based secondary prevention of overweight and obesity among 8- to 12-year old children: Design and sample characteristics of the SNAPSHOT trial
Abstract
Rising levels of severe obesity among children, worsening disparities by race and ethnicity and reluctance of primary care clinicians' to provide obesity management to children are compelling reasons to consider alternatives to primary care management of childhood obesity. The Students Nurses and Parents Seeking Healthy Options Together (SNAPSHOT) trial will test the efficacy of an elementary school-based, school nurse-led, healthy weight management program to reduce excess weight gain among children, 8- to 12-years old with a body mass index (BMI) 75th percentile, by increasing healthy dietary practices and physical activity and decreasing sedentary behaviors. SNAPSHOT has enrolled and randomized 132 child/parent dyads to either the: (1) 9-month SNAPSHOT intervention that includes four home visits, 14 kid groups held during out-of-school time and five parent groups or (2) a newsletter program consisting of monthly mailings and family-focused healthy lifestyle information. Outcomes are assessed at baseline, 12-months (post intervention) and 24-months (follow-up) post randomization. The primary outcome is child age- and gender-adjusted BMI z-score. Secondary outcomes include child dietary intake assessed with 24-h dietary recall interviews and accelerometer-measured activity levels. The SNAPSHOT intervention is a model of secondary obesity prevention for children that addresses the urgent need for theory-informed, evidence-based and safe weight management programs, delivered by skilled health professionals in accessible settings. This report describes development of the SNAPSHOT trial, including recruitment and randomization procedures, assessments, intervention and implementation plans, and baseline characteristics of the study sample.
Trial registration: ClinicalTrials.gov NCT02029976.
Keywords: Childhood obesity; Randomized controlled trial; Secondary obesity prevention.
Copyright 2018 Elsevier Inc. All rights reserved.
Publication types
- Clinical Trial Protocol
- Research Support, N.I.H., Extramural
MeSH terms
- Body Mass Index
- Child
- Diet*
- Exercise*
- Female
- Graphic Novels as Topic
- Humans
- Life Style
- Male
- Obesity Management* / methods
- Overweight / therapy
- Parents
- Patient Education as Topic
- Pediatric Obesity* / therapy
- Practice Patterns, Nurses'
- Randomized Controlled Trials as Topic
- School Health Services*
- School Nursing
- Screen Time
- Secondary Prevention
Associated data
- ClinicalTrials.gov/NCT02029976
School-based secondary prevention of overweight and obesity among 8- to 12-year old children: Design and sample characteristics of the SNAPSHOT trial
1.0.INTRODUCTION
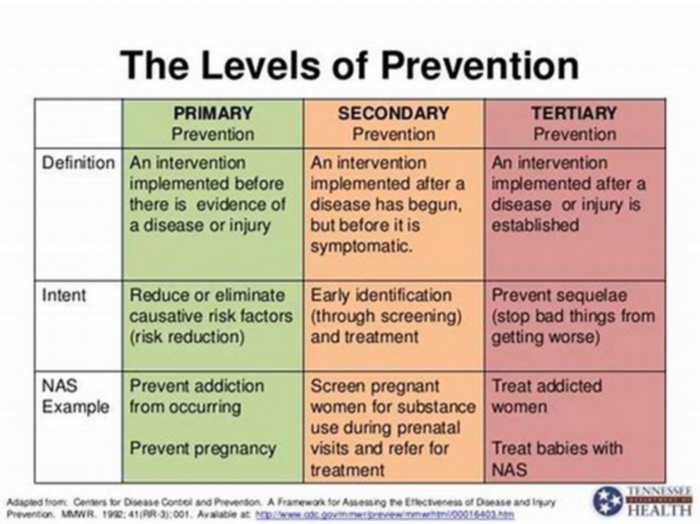
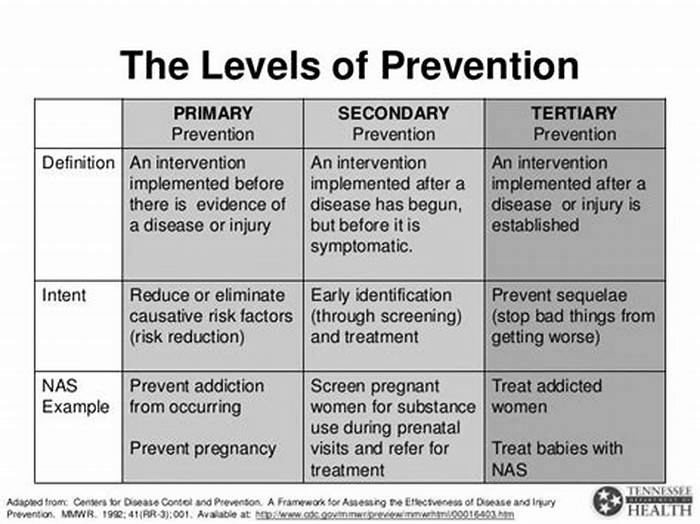
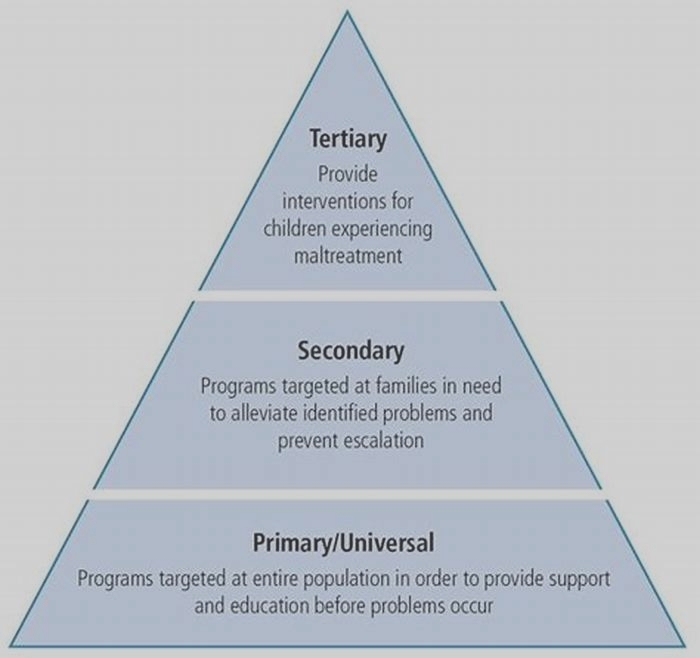
School-based interventions to influence childhood obesity and the weight-related behaviors of school-aged children have mostly tested primary prevention strategies to prevent the development of childhood obesity (1, 2). However, since more than one in three children is already overweight or obese (3), school-based programs that aim to prevent progression and support remission of childhood obesity or secondary prevention, merit consideration. Secondary prevention of childhood obesity typically occurs in primary care settings, where well disseminated recommendations from national experts guide practice (46). Recent gains in health insurance coverage for children have resulted in increased access and utilization of primary care services, especially among poor and near-poor families and black and Hispanic children (7). Yet the reluctance of primary care clinicians to provide obesity management and preventive services to children persist, with low rates attributed to training deficiencies, limited time and resources and reimbursement (811). Rising levels of severe obesity among children and worsening disparities by race/ethnicity, further complicate the situation and are compelling reasons to consider alternatives to primary care management of childhood obesity (3, 12).
Schools provide access to families with children, a familiar and accessible community setting to deliver programming and in many US school districts, licensed health professionals who are typically registered nurses (RN). School nurses are a large, highly skilled, RN work force underutilized in the fight against childhood obesity. Nationwide, nearly 95,000 RNs deliver school health services to more than 52 million children, with 82% of public schools employing a full- or part-time RN (13, 14). About one-half of school nurses are baccalaureate-prepared and 12% have a masters degree (14). Studies support school nurses interest in providing students obesity prevention services and suggest school nurse-delivered weight management programs are acceptable to parents (1519). Third-party payers already reimburse some school nursing services, and provide a financial model for reimbursement of obesity prevention programming (20).
Prior studies suggest school-based weight management programs are a promising approach (2123). However, treatment effects were offset by methodological concerns, including small sample size, variable duration of programming and lack of long-term follow up. Discussion of potential harms, such as unhealthy weight loss, weight teasing and bullying, which may be associated with weight management interventions was also missing from earlier studies. Consideration of unintended consequences is necessary when designing and implementing school-based weight management programs (24).
The Students Nurses and Parents Seeking Healthy Options Together (SNAPSHOT) study is the first to test in a full-scale randomized controlled trial, a school-based, school nurse-delivered healthy weight management program considerate of safety concerns, supportive of overweight and obese children and their families and sensitive to the strengths and limitations of the school setting. The SNAPSHOT intervention is a model of secondary obesity prevention that addresses the urgent need for effective, acceptable and safe weight management programming for children, delivered by skilled health professionals in accessible settings. The objective of this report is to describe the development of the SNAPSHOT trial, including recruitment and randomization, assessments, intervention and implementation plans, and baseline characteristics of the study sample.
2.0.METHODS
2.1. Study Design Overview
The SNAPSHOT study is a randomized controlled trial with random assignment of 8- to 12-year old children and a parent to the SNAPSHOT school nurse-delivered healthy weight management program (intervention condition) or a newsletter program (attention control condition). Cohorts or groups of children attending schools in one of two school districts located in the St. Paul/Minneapolis, Minnesota metropolitan area, along with their parent were recruited annually for four consecutive years from 2014 to 2017. Every year, following baseline measurement conducted from June to August, child/parent dyads within each cohort were randomized to a study condition, with post intervention and follow up measurement scheduled 12- and 24-months post randomization. Delivery of the intervention and attention control condition occurred during the 9-month school year, from September to May. The study was approved by the institutional review boards of Temple University (Philadelphia) and the University of Minnesota (Minneapolis).
2.2. Study Aims
The primary and secondary aims of the SNAPSHOT study are as follows:
Primary Aim: To test the efficacy of an elementary school-based, school nurse-led healthy weight management program to reduce excess weight gain among children, 8- to 12-years old with a body mass index 75th percentile, by increasing healthy dietary practices and physical activity levels and decreasing sedentary practices. We hypothesize that relative to the attention control condition, children receiving the intervention will have a significantly lower BMI, following implementation of the 9-month intervention, controlling for baseline values.
Secondary Aim 1: To examine the effects of the intervention on change in the weight-related behaviors of children. We hypothesize that the intervention will result in decreased consumption of sugar-sweetened beverages and energy-dense, low-nutrient foods, increased levels of moderate to vigorous physical activity, decreased sedentary behavior, and increased fruit and vegetable intake.
Secondary Aim 2: To examine the effects of the intervention on family lifestyle practices overseen by parents. We hypothesize that the effects of the intervention on family lifestyle practices overseen by parents, such as home availability of healthful foods, limits on screen time, frequency of family meals, will be more prevalent among families randomized to the intervention.
2.3. Study Sample
Children eligible for study participation were 8- to 12-years old, in second, third or fourth grade at the time of recruitment and attended an elementary school in one of two school districts that volunteered to participate in the study. One school district with a kindergarten through grade 12 enrollment of about 10,000 students is located in a suburban area, includes ten elementary schools, plus one parochial school and was a recruitment and intervention site from 20142017. The other school district with a kindergarten through grade 12 student enrollment of approximately 37,000 is located in an urban area, includes 43 elementary schools and was a recruitment and intervention site from 20162018.
Eligible children were required to have a BMI 75th percentile, calculated using the childs height and weight, as reported by the parent, school nurse or health care provider. Studies suggest that young children in the top quartile of the growth chart are at risk for excess weight gain during the early school years and intervention during this time may be critical to preventing excess weight gain (2527). Other inclusion criteria were child and parent able to read, write and speak English, child living with participating parent most of the time and willingness to be randomized to the intervention or the attention control condition. Exclusion criteria included plans to move outside the school district within the next 12 months, child with food allergies, physical limitations or medical conditions that would limit the childs ability to participate in physical activity and emotional health conditions that would limit the childs ability to participate in group activities with other children. Only one child per household was allowed to participate in the study.
All adult participants were required to provide written consent for self and child for study participation. Children were required to provide written assent. To allow time for review, consent forms were mailed to the parent prior to the baseline measurement visit. The consent process was completed at the first measurement visit and before baseline data collection.
2.4. Recruitment
Recruitment occurred each of four years from 2014 through 2017 and from January to June. Study staff identified recruitment strategies and developed materials that were reviewed and approved by school district administrators prior to use. For 2014 and 2015, recruitment occurred only in the suburban school district where elementary school students were provided annual height, weight and BMI screening, with all parents of participating children notified of results by mail. A form letter was added to this mailing that described the SNAPSHOT study and purpose, eligibility criteria and study participation details. Importantly, the letter stated that research staff did not have access to student height and weight information. A second mailing containing only the form letter was mailed a month later. The other school district joined the study in 2016 and did not provide students annual height, weight and BMI screening. Consequently, the form letter was discontinued and a recruitment flyer was developed and used in both districts. Colorful flyers of varying sizes depicted the SNAPSHOT comic characters who invited children and parents to join us for a research study with a focus on helping kids make healthy choices about food, being active & screen time, while having FUN! and included information on eligibility criteria and study participation. Across districts, flyers with tear-off tags that included the study phone number and email address were placed in high traffic locations in schools and community sites, such as libraries and park and recreation programs. Every month flyers were added to parent folders that were routinely used by classroom teachers and included materials for parent review that were hand-delivered by the child to the parent. A digital version of the flyer was posted on school and district websites. Throughout the recruitment period, study staff attended school events, such as family fun nights and parent-teacher conferences. In the suburban school district only, parents received a brief pre-recorded auto-call about the study from the school health services director once a month in April and May.
Interested parents were invited to call or email research staff for further information. Research staff arranged a convenient time to talk by phone with the parent and conduct eligibility screening. Once eligibility was established, the baseline measurement visit was scheduled.
2.5. Randomization
After baseline assessment, child/parent dyads within each cohort and school district site were randomized to receive the intervention or the attention control condition by the study statistician using a computer-generated randomization schedule (nQuery Advisor and nQuery Advanced v. 7 through 8.1.2.0, Statsols (Statistical Solutions Ltd), Cork, Ireland). School district sites were determined using the following parameters. Children attended different schools located throughout each school district, with school dismissal times assigned as early (3pm) or late (4pm) based on the districtwide busing schedule. With assistance from school district staff and considerate of school dismissal times and busing routes, centrally located school buildings were identified as school district sites where intervention delivery occurred. As a result, within each cohort and school district, there were typically two intervention groups. The one exception occurred in the suburban school district in 2016, when a uniform dismissal time for elementary schools was instituted, resulting in one intervention group.
2.6. Intervention
2.6.1. Logistics and Staff Training
The 9-month SNAPSHOT intervention is school-based, delivered during out-of-school time and includes four home visits with the parent/child dyad, 14 kid groups held once or twice monthly and five parent groups. Each intervention group was assigned to a trained research staff interventionist, a registered nurse licensed as a school nurse in Minnesota (hereafter referred to as school nurse interventionist) who delivered the intervention according to a standardized format. This approach facilitated consistency across different school nurse interventionists, multiple groups and cohorts. For the kid groups only, the school nurse interventionist was assisted with program delivery by trained research staff who were undergraduate nursing students. A key feature of the intervention was one school nurse interventionist delivered all program components to a group, which promoted trust and relationship building over time between the school nurse interventionist and child/parent dyad. Stability of kid and parent group membership facilitated development of rapport, trust and cooperation among group participants. Research staff received training in research with human subjects, motivational interviewing techniques, food safety and food preparation, group management and facilitation of games and other active play.
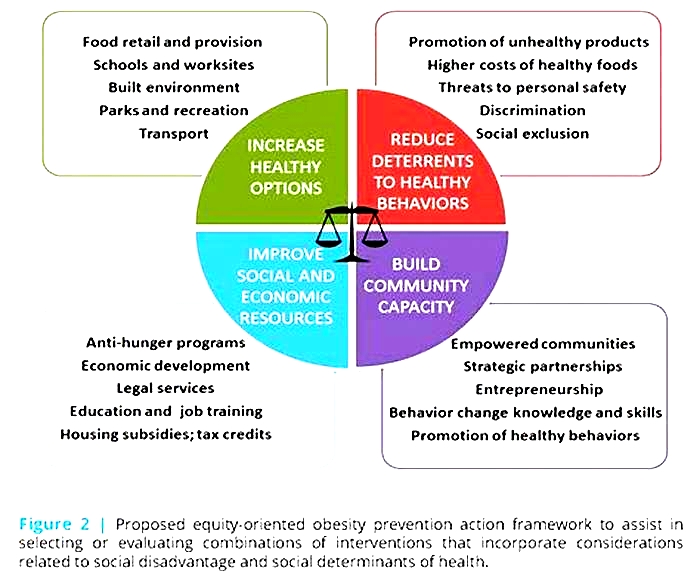
2.6.2. Conceptual Framework
A social ecological framework and the healthy learner model for student chronic condition management guided intervention design, implementation and evaluation (2831). Ecological models posit that key modifiers, which include intra- and inter-personal factors, social and cultural factors and the environment influence behavior (28, 29). Examples of personal factors are attitudes and beliefs about healthy weight management and self-efficacy to be physically active, choose healthy foods and limit sedentary activities. Behavioral factors include individual skill and intention to eat healthy foods and engage in regular physical activity. Environmental factors are defined as features of the physical environment that support, permit, encourage, or discourage participation in healthy food choice, physical activity, and sedentary activities. Social environmental factors include role modeling, normative practices and social support. Consistent with an ecological framework but specific to the school setting, the healthy learner model is an adaptation of the chronic care model that emphasizes care coordination for children with chronic conditions, overseen by a baccalaureate-prepared school nurse, with condition-specific expertise (3033). Nursing care is evidence-based, provided in partnership with the family and coordinated with the primary care provider and other community partners. See .
SNAPSHOT intervention: Conceptual Framework
2.6.3. Intervention Overview
The SNAPSHOT intervention is a multi-component healthy weight management program for 8- to 12-year old children that includes parents and targets key modifiable diet and activity factors known to be successful in changing long-term energy balance. Program content is consistent with the American Academy of Pediatrics obesity prevention guidelines and focuses on weight-related behaviors and lifestyle practices likely to help prevent excess weight gain in children and unlikely to cause harm (5, 34). These include: 1) consume 5 fruit and vegetable servings/day; 2) minimize sweetened beverages; 3) decrease screen time to 2 hours/day; 4) limit eating out, especially fast food restaurants; 5) eat breakfast daily; 6) encourage family meals; 7) limit portion sizes; and 8) be physically active 1 hour/day. The focus of the intervention is on supporting decision-making by the child, with an emphasis on healthy choice. The intervention balances the growing importance to the child of peers and increasing personal independence, the influence of parents considerate of parenting style, family dynamics, and cultural values, and the moderating effect of socio-demographic factors. provides an overview of the SNAPSHOT program. A full intervention dose consists of two contacts by the school nurse interventionist with the child and one contact with the parent every month. Descriptions of each program component follows.
Overview: The 9-month SNAPSHOT program
2.6.3.1. Home Visit
During the home visit, the school nurse interventionist provides the parent and child tailored support and guidance specific to self-identified goals and priorities for weight- related behavior change. The four visits occur at important transitions that include the new school year, which coincides with the beginning of the SNAPSHOT program; winter holiday break; spring break; and prior to summer vacation, which coincides with program completion. The transitions provide the theme for the 60-minute visit that follows an established template. This includes an icebreaker game; questions and review of the SNAPSHOT program content; a card-sort game that allows the child with parent assist to identify dietary and activity behaviors that are important to the child and a focus for behavior change; and a family goal setting activity led by child with parent assist. At the first home visit only, the school nurse interventionist collects a brief child health history and reviews procedures in case of accident or emergency during kid groups, as the parent is not in attendance. The school nurse interventionist also obtains permission from the parent to share with the childs primary care provider their participation in the SNAPSHOT study and intervention.
2.6.3.2. Kid Group
Research supports the effectiveness of group-based interventions for overweight and obese children and intervening with children and parents in separate groups (35, 36). The purpose of the SNAPSHOT kid group is to provide children guided learning, skill development and interactive play opportunities with a healthy eating and physical activity focus in a supportive group setting of similar-aged peers. Stability in research staffing and child participants over the 14 sessions contributed to the childrens comfort level with one another and the research staff, as well as a sense of support and safety within the group. To reinforce learning and skill development, a series of 14 comics, each with a targeted message about a healthy lifestyle practice were developed and provide the theme for each kid group. The comics are colorful and engaging, with behavioral messages conveyed in simple rhymes spoken by the SNAPSHOT comic characters, Nurse Karen Aboutkids, Trudy Foody and the Phyz, and comic villains such as Lord Bored (sedentary behavior), Sweatie Cheatie (sugary drinks), and the More Monsters (portion size). See for an example of the comics.
Examples of SNAPSHOT comics
Each 90-minute kid group followed an established template and included a welcome; review of group rules and goals from prior kid group; team building activity; a physical activity game; snack break with food preparation by each child; group read-aloud of the comic; hands-on behavioral activities linked to the comic theme; and individual goal setting. All groups included minimally 30 minutes of physical activity. At the completion of each group, children received a small incentive, valued at $1 or $2 and submitted their name for a grand prize drawing (YMCA one-week summer camp), held at the final kid group. Children who missed a group received the group materials by mail.
2.6.3.3. Parent Group
Parent involvement in programs to affect child weight is critical, especially for younger children (37, 38). The purpose of the SNAPSHOT parent group is to provide parents peer support, feedback and information sharing in a supportive parent-friendly setting. The five, 90-minute groups are led by a school nurse interventionist and scheduled during the months home visits are not scheduled (October, November, January, February, April). The early evening sessions followed an established template that included: a welcome and icebreaker activity; a light easy-to-reproduce dinner prepared in advance by the school nurse interventionist; review of group guidelines; family check-in to monitor progress with family and child goals; a team-building activity; SNAPSHOT program review; and two behavioral activities that mimicked the content provided children in kid group, thus reinforcing behavioral messages across parent and child groups. Similar to the kid groups, all parent groups included minimally 30 minutes of physical activity. At the completion of each group, parents received a small incentive, valued at $2 or $3 and submitted their name for a grand prize drawing, ($50 farmers market gift certificate) held at the final parent group. Parents who missed a group received group materials by mail.
2.7. Attention Control Condition
Child and parent dyads randomized to the attention control condition received a newsletter program consisting of monthly mailings that contained healthy lifestyle information for the family. There were also recommendations for community-based family fun events scheduled during the month with an activity focus and a healthy easy-to-make recipe. Lifestyle information addressed a variety of topics such as bike safety, immunizations, dental health, bullying, car safety and family first aid.
2.8. Assessment and Outcome Measures
Data collection was performed by trained research staff using standardized procedures, and occurred at baseline prior to randomization, and 12- (post intervention) and 24-months (follow up) post randomization. Two person teams conducted measurement at a centrally located school district building or the participants home, based on parent preference. The baseline and post intervention measurement required 90 minutes; the follow-up visit at 24 months post randomization required 60 minutes. At each measurement, the parent received a $75.00 gift card and the child received a $50.00 gift card.
2.8.1. Child and Parent Anthropometry
BMI is the recommended method of assessing overweight among adults and children and is calculated with the formula: weight (kg)/[height (m)2] (39). Research staff collected child and parent height and weight using standardized procedures (40). BMI percentiles and BMI z-scores for childs gender and age were calculated using the 2000 Centers for Disease Control and Prevention (CDC) growth charts. The studys primary outcome measure was child age- and gender-adjusted BMI z-score. We also measured parent and child body fat percentile using a Tanita TBF-300A body composition analyzer scale. All anthropometric measures were collected at baseline, post intervention and follow-up.
2.8.2. Child Dietary Intake
Child dietary intake was assessed with multiple 24-hour dietary recall interviews, considered the gold standard for assessing dietary intake (41). At baseline and post intervention, trained and certified staff conducted two phone interviews with the child (one weekday and one weekend day) using the multiple pass method (42, 43). Parental assistance was permitted for clarification (44). Recalls were collected and interpreted using the Nutrition Data Systems for Research (NDS-R) nutrient calculation software (45). Additional information collected during the interview included the childs eating companions, the location of the meal and use of screens while eating.
2.8.3. Child Physical Activity
Child physical activity was assessed at baseline and post intervention with the ActiGraph uniaxial accelerometer, validated for use in children (4648). The ActiGraph was worn at the right hip for a 7-day period; four days of complete data were required for analyses (49). Counts were classified into intensity categories of sedentary, light, moderate, vigorous and moderate to vigorous physical activity (MVPA) using age appropriate count cutoffs (50, 51). We also calculated number and average length of MVPA bouts. Trained research staff fit the Actigraph to the child, as per standard protocols (46, 52).
2.8.4. Child Health-related Quality of Life
Health-related quality of life (QOL) has shown an inverse association with obesity among children (23, 53). We used the 23-item pediatric QOL inventory, PedsQL 4.0 to assess physical, emotional, social and school functioning (54). The inventory takes four minutes to complete and is reliable and valid in school-aged children (55, 56). The children completed the inventory independently as part of the child survey. Parents completed the parallel parent proxy report as part of the parent survey. The inventory was collected at baseline, post intervention and follow-up
2.8.5. Psychosocial Factors
Psychosocial factors serve as predictors and mediators of behavior change and were assessed via paper and pencil surveys administered at baseline, post intervention and follow-up and completed independently by child and parent. An example of items included on the child survey and used successfully in previous studies with similar aged children were intentions to eat healthy food at school; self-efficacy to eat healthy; barriers to healthy eating; physical activity self-efficacy; and physical activity self-management (57). Psychosocial and environmental mediators at the family level were included on the parent survey. Examples of scales included parent motivation for healthy eating; self-efficacy for healthy food preparation; support and modeling of healthy eating; parent motivation for physical activity with child; and self-efficacy for physical activity with child (5860).
2.8.6. Other Survey Items
The parent survey also included child and parent demographic information, such as gender, race, ethnicity and birthdate of participating child and parent. Parents self-reported their education, marital and employment status, household family structure, household income, eligibility for the free and reduced lunch program and household food insecurity. Items about parent and child health problems, perceived health of parent and child, frequency of child visits to health care provider and frequency of missed work by adults in the household due to child illness were assessed. The child completed a 5-item pubertal development scale shown to be reliable when compared to interviewer and physician ratings (61).
Parents self-reported their dietary, physical activity and sedentary practices. Measures included a validated 17-item fat screener and 6-item fruit and vegetable screener, as well as single items to assess sweetened beverage consumption, fast food restaurant use, breakfast consumption, and frequency of family meals (41, 62, 63). Parent physical activity was measured with a modified version of the Godin and Shepard Leisure Time Exercise Questionnaire; other survey items assessed weekday and weekend sedentary behaviors and parent rules related to child media use (6466).
2.9. Process Measures
Comprehensive process evaluation provides important information about several aspects of a randomized controlled trial, including recruitment, assessment and intervention dose, reach, context and fidelity (67, 68). provides an overview of the process data collected.
Table 1.
SNAPSHOT Trial: Overview of Process Measures
| Component | Data Collected | Method | Category |
|---|---|---|---|
| Recruitment | Type strategy and use | Recruitment log | Context |
| Exposure to strategy | Recruitment Survey | Dose, Reach | |
| Measurement | Location | Measurement log | Context |
| Reminders | Measurement log | Context | |
| Intervention: | |||
| - Home Visit | Attendance | Attendance log | Reach; Dose; Fidelity |
| - Kid Group | Components completed | Session process form | Fidelity |
| - Parent Group | Handouts | Archive of printed materials | Context |
| Intervention: Participant Satisfaction | Child-reported satisfaction | Kid Satisfaction Survey | Reach; Context |
| Parent-reported satisfaction | Parent Satisfaction Survey | Reach; Context | |
| Cost of Intervention Delivery | Food | Receipts | Context; Reach |
| Equipment | Receipts | Context; Reach | |
| Paper supplies | Purchase Orders | Context; Reach | |
| Mailing costs | Mailing log | Context; Reach | |
| Busing | School district invoices | Context; Reach | |
| New sletter Program | New sletters mailed | Mailing log | Reach; Dose; Fidelity |
| Content of new sletters | Archive of newsletters | Context |
2.10. Statistical Analysis
The primary outcome is child age- and gender-adjusted BMI z-score. at post-intervention that will be compared between intervention and attention control groups. Generalized Linear Mixed Models (GLMM) will be used to model partial clustering of the data and to account for potential intra-class correlation that may develop within the intervention sub-groups. We will also explore an adjustment for a priori selected baseline factors known to be associated with the primary outcome such as child age, gender, race, ethnicity and receipt of economic assistance. For exploratory analyses, we plan to assess potential differences in the primary outcome over time using GLMM with group and assessment time point as fixed covariates, while controlling for partial clustering and for the baseline factors of interest, as needed. This approach accounts for correlation between repeated measures taken over time, accommodates missing data and provides reliable estimates using all available data. Outcomes associated with secondary aims, including child body fat percentile, dietary intake, Actigraph and QOL will be analyzed utilizing the same model used for the primary outcome, adjusting for relevant covariates of interest.
Intervention dose will be examined among intervention participants only. The actual implemented dose will be correlated with the observed BMI z-score changes. Magnitude and pattern of missing data will be examined, and expected and observed attrition rates will be compared. A mixed model-based approach will be used to handle realized missing data. Sensitivity analysis will also be explored. A two-sided type I error rate of 5% (in conjunction with the two-sided 95% confidence intervals) will be used to assess statistical significance.
2.11. Sample Size Considerations
The sample size calculation for the primary outcome was based on the sample size formula for baseline-adjusted analysis of covariance (with the baseline value of the primary outcome as covariate), and a two-sided type I error rate of 5% at 12-months post randomization, following intervention completion. The variance estimate used in the formula was adjusted for correlation between the baseline and post-intervention measurements and for clustering in the intervention group (69). Estimates of over-time correlations of BMI z-scores (r=0.80.97) were based on data from the HOME pilot study that included similar aged children (70). Population standard deviation of BMI z-scores is about one. Using an assumed correlation of 0.88 between BMI z-scores over time, and a conservative standard deviation of BMI z-scores of about 0.7 (supported by simulation results), we expect to detect an effect size of 0.25 for age- and gender-adjusted BMI z-scores at 80% power with a sample size of 114 children. Using the BMIi = M(1+LSzi)1/L formula with age-and gender-specific L, M, S parameters and 50th percentile for height values for 8- to 12-year old children, this effect size translates to an estimated 1.7 kilogram (3.74 pound) decrease in average weight gain for boys and girls between intervention and attention control conditions at post intervention (71). Recruitment of 132 child/parent dyads allowed for an attrition rate of 15% and a final effective sample of 114 dyads or 57 dyads per condition.
2.12. Data Safety and Monitoring Plan
The SNAPSHOT trial is not a weight-loss study. The study aims to reduce excess weight gain among school-age children 8- to 12-years old. The focus is not on weight loss or decreasing energy intake. Rather, healthy eating practices such as consuming fewer high-fat foods and sugary drinks and increasing fruit and vegetable intake are promoted. The intervention goals of 60 minutes of physical activity a day and reducing minutes spent in sedentary activity are consistent with national recommendations (66). During the 9-month intervention, the school nurse interventionist has twice-monthly contact with parents and children in a group setting or during the one-on-one visit with the parent and child dyad. This provides an opportunity for ongoing assessment of a childs general health, both physical and emotional and any parent concerns.
The intervention is not associated with any direct risks to the child. Since an increase in frequency and duration of physical activity may lead to an increase in minor injuries such as abrasions and strains, injury occurrence was monitored. It is possible although not considered likely that a child may experience a change in weight and/or height during the 9-month intervention period considered outside an acceptable range. As a safety precaution, height and weight were collected approximately midway between the baseline and post intervention measurement on all children. Values considered below a pre-set cutoff, based on expected 6-month incremental growth for weight and stature by child age and gender, triggered review by the study pediatrician to determine if parent notification and follow up with the primary care provider was indicated (72). At the school level, to address the potential negative consequences of a school-based weight management intervention, a web-based educational module was developed and provided to the participating school districts. The module was not a part of the intervention but rather a health-related service provided to the school districts. The module, entitled Preventing Weight Stigma targeted parents and school staff, influential adults identified as a source of weight bias toward children. Few efforts to reduce stigma among overweight and obese children have addressed adults (24).
3.0.RESULTS
depicts the results of recruitment, eligibility determination and enrollment that occurred from 2014 through 2017. Among the 235 dyads completing screening, 88 did not meet eligibility criteria. The most common reasons for child ineligibility included BMI percentile <75th (n=42), not in required grade (n=10), food allergy (n=10), moving out of the school district (n=9) and school not a study school (n=8). Among the 147 dyads that met eligibility criteria, 132 dyads (90%) agreed to study participation, provided consent, completed baseline measurement and were randomized to receive either the intervention condition (n=66) or the attention control condition (n=66).
SNAPSHOT flow diagram of participant screening, eligibility and enrollment
shows baseline characteristics of the child and parent participants by condition. Overall, children have a mean age of 9 years, slightly more than half are boys and the majority are non-White (63%). About half of the children are obese and 27% are overweight. Among parents, the mean age is 39 years. Almost all are female (94%) and less than half are non-White (42%). Although most (83%) reported some college, well over half (59%) received economic assistance. Among parents, nearly one-half are obese and 27% are overweight.
Table 2.
Baseline characteristics of child and parent participants, by condition
| Total Sample(n=132) | Intervention(n=66) | Control(n=66) | |
|---|---|---|---|
| Child Characteristics | |||
| Age (M, SD) | 9 (0.9) | 9 (0.9) | 9 (0.9) |
| Gender (% Male) | 67 (51%) | 32 (48%) | 35(52%) |
| Race/Ethnicity | |||
| White | 49 (37%) | 24 (36%) | 25 (38%) |
| Hispanic | 30 (23%) | 15 (23%) | 15 (23%) |
| Black | 28 (21%) | 13 (20%) | 15 (23%) |
| Other | 25 (19%) | 14 (21%) | 11 (17%) |
| BMI z Score (M, SD) | 1.6 (0.67) | 1.5 (0.65) | 1.7 (0.68) |
| Weight Status | |||
| BMI% < 85th | 29 (22%) | 19 (29%) | 10 (15%) |
| 85th% BMI% <95th | 36 (27%) | 19 (29%) | 17 (26%) |
| 95th | 67 (51%) | 28 (42%) | 39 (59%) |
| % Body Fat (M, SE)1 | |||
| Girls | 32.6 (1.12) | 31.7 (1.55) | 34.0 (1.60) |
| Boys | 28.6 (1.27) | 26.3 (1.51) | 30.4 (1.94) |
| Pubertal development (M, SD)2 | |||
| Girls | 1.8 (0.58) | 1.7 (0.59) | 1.9 (0.56) |
| Boys | 1.6 (0.42) | 1.5 (0.32) | 1.6 (0.47) |
| Parent Characteristics | |||
| Age (M, SD) | 39 (7.1) | 39 (7.4) | 39 (6.7) |
| Gender (% Female) | 124 (94%) | 63 (96%) | 61 (92%) |
| Race/Ethnicity | |||
| White | 76 (58%) | 40 (61%) | 36 (55%) |
| Black | 26 (20%) | 12 (18%) | 14 (21%) |
| Hispanic | 17 (13%) | 9 (14%) | 8 (12%) |
| Other | 13 (10%) | 5 (8%) | 8 (12%) |
| Weight Status | |||
| BMI < 25 | 34 (26%) | 19 (29%) | 15 (23%) |
| 25 BMI < 30 | 35 (27%) | 17 (26%) | 18 (27%) |
| BMI 30 | 63 (48%) | 30 (46%) | 33 (50%) |
| % Body Fat (M, SE)3 | |||
| Female | 37.9 (0.85) | 37.4 (1.06) | 38.4 (1.34) |
| Education | |||
| high school | 23 (17%) | 10 (15%) | 13 (20%) |
| Some college | 35 (27%) | 18 (27%) | 17 (26%) |
| Associate degree | 21 (16%) | 12 (18%) | 9 (14%) |
| Bachelors degree | 53 (40%) | 26 (39%) | 27 (41%) |
| Economic assistance (% Yes) | 78 (59%) | 41 (62%) | 37 (56%) |
4.0.DISCUSSION
Since 20072008, trends in obesity prevalence among 6- to 11-year old children show a leveling off at about 17%; in contrast, rates of severe obesity are on the rise and currently affect 4.5 million or 6% of children 2- to 19-years of age (12, 73). Severe obesity is strongly associated with an increased risk of cardiovascular and metabolic risk (74). Using current rates of childhood obesity, modeling studies predict that over one-half of todays children, and particularly those with severe obesity, will be obese by age 35 (12). Engagement by primary care providers in childhood obesity prevention continues to fall short of recommended practice (811). A few primary care-based obesity intervention trials targeting children have shown modest results, yet, concerns about translation and implementation in busy practice settings have been expressed (75). Alternatives to clinic-based care merit consideration if progress in resolving the childhood obesity epidemic is to occur.
The National Institutes of Health strategic plan for obesity research calls for accessible, cost-effective interventions that test new approaches to reach and maintain a healthy weight among diverse populations, in real world settings (76). In the US, schools remain the best venue for reaching children and families, independent of race, ethnicity, income and geography. Providing healthy weight management programs in concert with schools and school nurses provides children and families access to a familiar safe space in a child- and family-friendly community setting and a trusted, qualified health professional, experienced at facilitating links between families, health care providers and community resources. Effective interventions that result in improvement in weight status among children with obesity must be comprehensive, and typically require 26 contact hours (77). Physical facilities needed to support diet and activity interventions include indoor and outdoor play spaces and food preparation and dining facilities are common in schools and usually made available at no or minimal costs to school groups for out-of-school programming that requires multiple sessions over an extended period. The SNAPSHOT study is the first fully powered randomized controlled trial to design, implement and evaluate a school nurse-delivered healthy weight management program to reduce excess weight gain among 8- to 12-year old children with a BMI 75th percentile. Trial success and potential for translation and scalability is enhanced by: a rigorous study design; intervention development and implementation that is theory- and evidence-based; consideration of potential safety concerns, both physical and emotional and procedures to prevent and monitor occurrence; process data collection to document fidelity, context and reach; and prospective economic analysis to inform sustainability and a framework for reimbursement. We anticipate that SNAPSHOT will be a new model of secondary obesity prevention, with potential for dissemination in schools nationwide.