What dog breeds are more prone to pancreatitis
Pancreatitis in Dogs Symptoms, Causes & Treatment
Pancreatitis in dogs is one of those conditions that owners must be informed about before it strikes because the warning signs may not always be obvious at first, the symptoms might be mistaken for something less serious, and yet its potentially life-threatening. The medical definition of pancreatitis is simple: inflammation of the pancreas. But like all serious conditions, there is more to it than that.
Because it is dangerous, a suspected case of pancreatitis needs to be addressed by a veterinarian as quickly as possible and not dealt with by DIY treatments. As with all medical issues, even the best online resource is not a replacement for the medical guidance from your vet.
Before looking at the details of pancreatitis, lets take away the ititis and explain the small but vital organ itself:
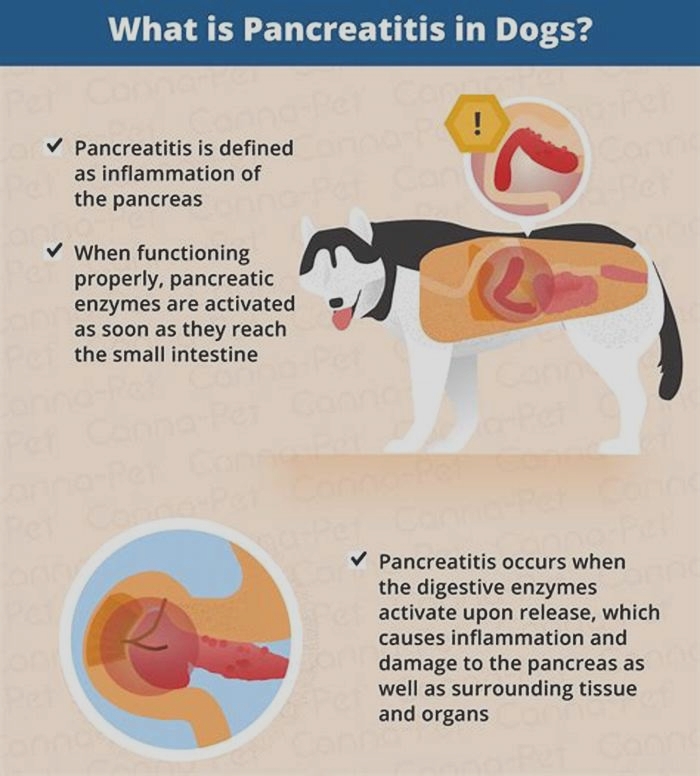
The pancreas is responsible for releasing enzymes that aid in digestion. When the organ is working normally, the enzymes become active only when they reach the small intestine. In a dog with pancreatitis, however, the enzymes activate when theyre released, inflaming and causing damage to the pancreas and its surrounding tissue and other organs. According to the Whole Dog Journal, the enzymes can actually begin to digest the pancreas itself, which causes extreme pain to your dog.


Classic signs of pancreatitis in dogs
- Hunched back
- Repeated vomiting(either several times within a few hours or periodically over several days)
- Pain or distention of the abdomen (dog appears uncomfortable or bloated)
- Diarrhea
- Loss of appetite
- Dehydration
- Weakness/lethargy
- Fever
If your dog exhibits one of these signs, and only infrequently, monitor her. But if she exhibits multiple signs at once, and repeatedly, a call to the veterinarian quickly is vital.
Dehydration and pancreatitis in dogs
Dehydration is due to a greater fluid loss than fluid intake. Diarrhea or vomiting can cause dehydration, but those signs together will cause a greater fluid deficit and dehydration because the dogs fluid input (drinking) cannot keep up with the fluid losses. If the diarrhea becomes bloody, the condition worsens and the dehydration can become an emergency.
Other factors such as fever require increase fluid intake and can lead to dehydration along with other metabolic issues such as kidney disease, etc.
Blood in a dogs stool indicates a loos and significant inflammatory response requiring a veterinarians attention but it can be cause by a multitude of factors, from ulceration to parasites. Dehydration is a serious condition that can lead to death. It is an emergency and requires immediate veterinary care.
Any lethargic dog who is not drinking water or cannot hold water down should be suspect of dehydration and examined by a veterinarian. Dry mucous membranes (such as gums) may be a quick way of assessing dehydration but as always, when in doubt, consult with your veterinarian.
Causes of pancreatitis in dogs
There are a number of causes and risk factors that can bring on pancreatitis. Though often the attack appears seemingly out of the blue. Among them are:
- A high-fat dietThis is a major cause of pancreatitis, especially for a dog who gets one large helping of fatty food in one sitting
- A history of dietary indiscretion (a medical term for saying your dog will eat anything)
- Obesity
- Hypothyroidism (or other endocrine diseases)
- Severe blunt trauma
- Diabetes mellitus
- Certain medications or other toxinsThese include cholinesterase inhibitors, calcium, potassium bromide, phenobarbital, l-asparaginase, estrogen, salicylates, azathioprine, thiazide diuretics, and vinca alkaloids.
- There may, in some cases, be a genetic predisposition. Certain breeds or types of dogs have been associated with higher risks of pancreatitis such as Miniature Schnauzers and some of the smaller toy and terrier breeds.
More about those fats: Human food is especially dangerous, though even high-fat dog food may cause pancreatitis. So owner vigilance is particularly required around holidays and other festive occasionsthey can bring well-meaning guests who slip your buddy a fatty piece of lamb, or a tray of buttery cookies left within reach of an eager muzzle. In fact, the day after Thanksgiving is known for more than just Black Friday bargains. Its one of the busiest days of the year pancreatitis-related emergency vet visits.
Basically, if your dog is showing any signs of abdominal pain, the worst thing to do is feed him a fatty diet. This is one of many reasons that giving your dog table scraps, as tempting as it may be, is not advisable.
How does a vet diagnose pancreatitis in dogs?
- Your dogs medical history
- Blood tests to measure pancreatic enzymes
- Physical examination including stomach, gums, heart, temperature
- Radiographs or ultrasound, to rule out other causes
- Fine needle aspiration of the pancreas
As the Merck Veterinary Manual notes, as with any disease, no test should be used in isolation for diagnosis, and all clinical findings should be used in conjunction to arrive at the most appropriate diagnosis.


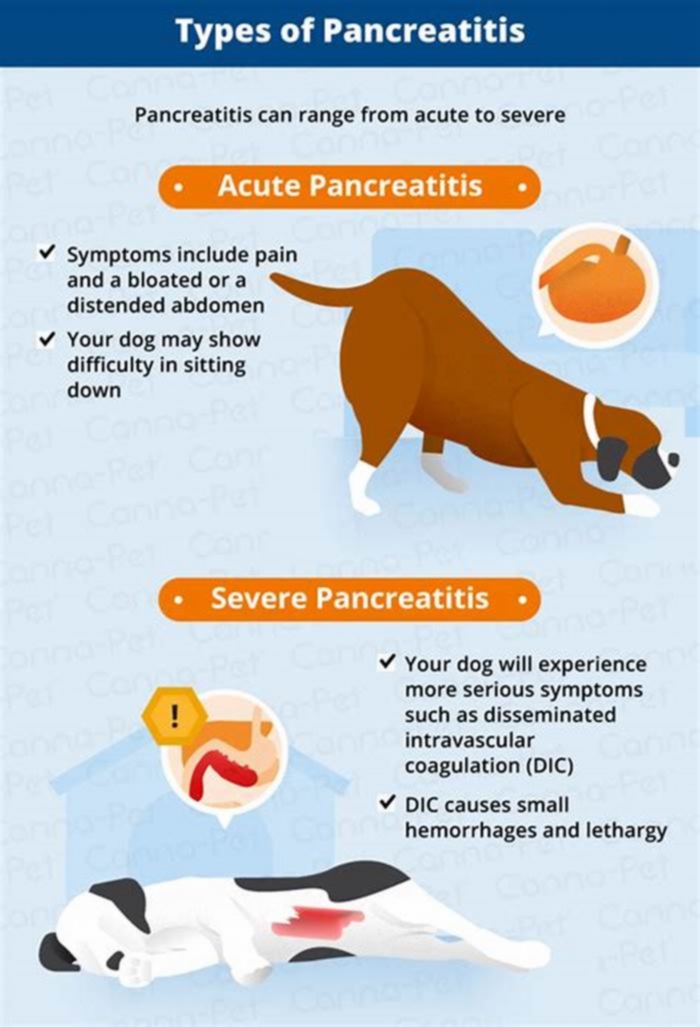
Whats the difference between acute and chronic pancreatitis?
Acute PancreatitisAn acute attack of pancreatitis means it comes on suddenly, with no previous appearance of the condition before. It can become life threatening to other organs if the inflammation spreads.
Chronic PancreatitisA chronic condition is one that has developed over time, slowly, and often without symptoms. This condition can result from repeated bouts of acute pancreatitis.
Both acute and chronic forms can be either severe or mild, and both result in pain.
Treatment and management of pancreatitis in dogs
Theres no fancy treatment for acute pancreatitis. First and foremost, your dogs pain must be managed, and early intervention to prevent further complications is key. The most common treatment and management options are:
- Intravenous (IV) fluid therapy in severe pancreatitis
- Vigorous monitoring of a worsening condition
- Antiemetic medication for vomiting (to prevent dehydration)
- Resting the pancreas (withholding food and water for 24 hours)Long-term management includes:
- Vigilant monitoring of fat intakeNo table scraps allowed!
- Use of a prescription diet of gastrointestinal-supportive low-fat, or ultra-low fat, food.
- Feed smaller, more frequent meals instead of one larger meal
- Have amylase and lipase levels checked by a veterinarian regularly
Can supplements be used to prevent or manage pancreatitis in dogs?
It is important to reiterate that pancreatitis is a serious condition, so home remedies shouldnt be used in place of veterinary intervention. That said, some vets believe digestive enzyme supplements with pancreatin can help some (not all) dogs by reducing the work of the pancreas and inhibiting pancreatic secretion. These come in over-the-counter strength as well as prescription strength.
Fish oil may seem counterintuitive at first, because of its high fat content, but it can actually help lower blood lipid levels. Studies suggest a high level of fish oil (about 1,000 mg. per 10 pounds of body weight for dog with high lipid levels; about half that amount for dogs with normal levels) is helpful to dogs with acute pancreatitis. When supplementing with fish oil, also supplement with 5 to 10 IU of vitamin E.
There have been human studies suggesting that vitamin E (with selenium), vitamin C, beta-carotene, and methionine may help prevent pancreatitis. Conversely, another human study reveals that probiotics can make acute pancreatitis worse.
Always speak with your veterinarian before offering any supplements to your pet.


A canine researchers case study: her own dog
Caroline Coile, Ph.D is the Nutrition and Health columnist for AKC Family Dog and a two-time AKC Canine Health Foundation Award winner. Pancreatitis is a subject Coile knows well, not only as a professional canine researcher and writer, but because her dog, a Saluki named Beanie, went through the difficult and stressful experience. Here she shares her story:
Beanie, unlike most Salukis, loves to eat. But one day, after eating his very favorite treata flaky biscuithe vomited it up. He was standing with his back kind of hunched. I gently pressed on his abdomen, and he yelped. Out came the thermometer, which told me his temperature was 103 degrees. While I was calling the veterinarian, he vomited again, then lay down in a corner. We were in the car within minutes.
The veterinarian palpated his abdomen, which was definitely tender; took his temperature, which was still high; and drew blood. Beanie received pain medication, antibiotics, and intravenous fluids to combat fluid loss and came home with strict instructions not to eat that day. Eating anythingor even smelling foodcould have caused his pancreas to secrete enzymes and slow its healing. He could lick ice cubes, and then drink a bit of water.
The next day, he was allowed to eat about six tiny meals of low-fat, high-carbohydrate food. This meant rice, potatoes, or pasta. Overcooking these starchy foods makes them easier to digest. We would boil one cup of white rice (not instant rice) in four cups of water for 30 minutes to make a rice porridge called congee. We gradually added in protein sources, such as skinless chicken breast, low-fat cottage cheese, or boiled hamburger meat. When feeding a dog with pancreatitis, its important to cook all the food even if you normally feed a raw diet. Because the dogs gut is compromised, its necessary to remove fat and destroy bacteria.
After a week, Beanie progressed to a veterinary prescription diet for dogs with pancreatitis. He hated it. Many dogs with a history of acute pancreatitis must be on a special diet for the rest of their lives. If they dont like the pancreatitis diet, a low-fat weight loss diet often works just as well. Since obese dogs are more prone to pancreatitis, they need to lose weight anyway. Even if a high-fat meal didnt cause the initial bout, it can trigger a recurrence once the dog has had pancreatitis.
After a month, Beanie was able to gradually transition back to his old diet, minus the high-fat treats. Eventually, he even got his breakfast biscuitsbut no more butter. He never had another bout of pancreatitis.
The Take-Away
As the Canine Journal puts it, pancreatitis is like that relative that just wont leave: Even when theyre gone, the thought of their return hovers in the back of your mind. Unfortunately, once a dog has had a bout of pancreatitis, the chance of recurrence is high. You best defense against a repeat appearance of this unwelcome intruder is a two-pronged approach: Be on the look-out for the warning signs and control the things you can. Dont let your dog become obese (exercise is good for both of you), follow your vets feeding instructions strictly, and, when relevant, administer your dogs medication faithfully.
Mild cases of pancreatitis usually have a good prognosis. Severe cases have a more guarded prognosis, due to the potential for systemic complications. But as a vigilant, responsible, and most of all, knowledgeable dog owner, you now know what you can do to reduce the risk of pancreatitis, how to recognize it if it does strike, and how to manage it going forward.
What Causes Pancreatitis in Dogs and How to Treat It
If you have a dog thats predisposed to pancreatitis, or one that tends to sneak fatty foods when youre out on a walk, you might want to know more about the symptoms and treatment of pancreatitis in dogs.
Heres what you need to know about pancreatitis in dogs so you can have a better understanding of this condition.
What Is Pancreatitis in Dogs?
The pancreas is an organ in the abdominal cavity. One of its roles is producing digestive enzymes, which helps break down food products.
Pancreatitis in dogs is an inflammatory reaction within the pancreas that can result in abdominal pain, inappetence, and vomiting.
The inflammation results from the inappropriate, early activation of an enzyme within the pancreas, which causes the pancreas to digest itself.
What Causes Pancreatitis in Dogs?
Classically, the typical history of a canine patient that is diagnosed with pancreatitis is one in which the dog ate a high-fat meal or got into the garbage. Unfortunately, this is not the most common cause of pancreatitis.
In reality, 90% of the time, the inciting cause of pancreatitis in dogs is idiopathic (cannot be determined).
Are Some Dogs Predisposed to Pancreatitis?
Some breeds are more prone to the development of pancreatitis, as well as dogs taking certain medications.
Miniature Schnauzers are considered to be a predisposed breed due their tendency to have problems with high blood triglyceride levels.
Another example is the English Cocker Spaniel. Immune-mediated diseases, which result from abnormal activity of the immune system, are seen at a higher frequency in this breed in general, and the immune system attacking the pancreas is no exception.
Medications that are known to cause inflammation of the pancreas include, but are not limited to, some chemotherapy medications and some antibiotics.
What Are the Symptoms of Pancreatitis in Dogs?
Pancreatitis can present as a sudden-onset (acute) illness or as a more long-term (chronic) illness.
A dog that has acute pancreatitis will have more serious clinical signs, such as:
A dog with chronic pancreatitis is typically not as sick. The clinical signs may include:
In general, chronic pancreatitis is not as common in dogs as acute pancreatitis.
Dogs with chronic pancreatitis can suddenly develop worsening pancreatitis. This is a situation where chronic pancreatitis presents acutely.
How Do Vets Diagnose Pancreatitis in Dogs?
Disease of the pancreas can be difficult to identify because, oftentimes, the signs of illness are not specific to the pancreas, and routine blood tests are often not helpful.
However, there are pancreatic-specific blood tests that can be performed when the veterinarian has a high suspicion of pancreatitis.
Unfortunately, even these special tests are not 100% accurate.
Abdominal X-rays are also not very helpful in diagnosing pancreatitis in dogs. However, in a vomiting patient, it is important to take X-rays to rule out a potential foreign-body obstruction of the stomach and/or intestine (something your dog ate, like a squeaker out of a toy).
The best method to image the pancreas is via abdominal ultrasound. However, the tissue of the pancreas has to be abnormal enough to visualize using the ultrasound, which is more common in dogs with acute, severe pancreatitis, when compared to those with chronic, mild pancreatitis.
Overall, blood testing and abdominal ultrasound are better in helping to diagnose pancreatitis in dogs when it is acute and severe.
How to Treat Pancreatitis in Dogs
Treatment is primarily supportive care regardless of whether the patient has acute or chronic pancreatitis.
Severe Pancreatitis in Dogs
Patients with severe, acute pancreatitis often require more extensive medical intervention and treatment.
These patients are often in need of several days, if not weeks, of treatment, including:
Intensive intravenous (IV) fluid and electrolyte support
Pain-control measures
Antinausea medication(s)
Stomach-protectant medications
Nutritional support in the form of a feeding tube
Antibiotics (sometimes)
Severe pancreatitis patients are often critical and best treated in a specialist practice, such as an intensive 24-hour care facility. The cost for treatment is estimated at approximately $2000-5000 but can vary depending on where you live.
Moderate to Mild Pancreatitis in Dogs
Patients with moderate or mild pancreatitis may be hospitalized for one to a few days for IV fluid therapy to correct dehydration.
In a dog with mild pancreatitis, your veterinarian may determine that subcutaneous (applied under the skin) fluid administrationeither at the appointment or at homewill be adequate for rehydration.
These patients are usually also treated with:
In general, mild to moderate pancreatitis patients recover in one to two weeks. Treatment can vary with these patients, so the cost varies. If hospitalized for a few days, the costs can approximate $1500-2500. If treated as an outpatient, the cost is around $500-1000.
A permanent diet change may be recommended, especially in predisposed breeds (Schnauzers) or dogs with a previous history of pancreatitis.
What Is the Prognosis for Pancreatitis in Dogs?
The prognosis for dogs with pancreatitis ultimately depends on the severity of the illness.
A dog with severe pancreatitis has a poor to grave overall prognosis, thus a higher risk of death. These patients can die from a severe whole-body inflammatory condition, which results in multiple organ failure.
Pancreatic abscess formation and peritonitis (abdominal cavity infection) is another complication of severe pancreatitis that increases the risk of fatality.
It is important to note that a dog that has recovered from even a single episode of pancreatitis or repeated episodes of pancreatitis may develop extensive scarring within the pancreatic tissue.
This can lead to the development of diabetes mellitus and/or a condition called exocrine pancreatic insufficiency (EPI). EPI occurs as a result of the pancreas not being able to produce a sufficient amount of digestive enzymes.
Pancreatitis has many potential causes, and dogs can present with illness that ranges from mild to very severe. Also, the signs of illness are not specific to the pancreas, so it can be a challenge to diagnose. Ultimately, the earlier the diagnosis and treatment, the more positive the outcome.
Featured Image: iStock.com/Elen11