What are the solutions to obesity in society
What Can Be Done
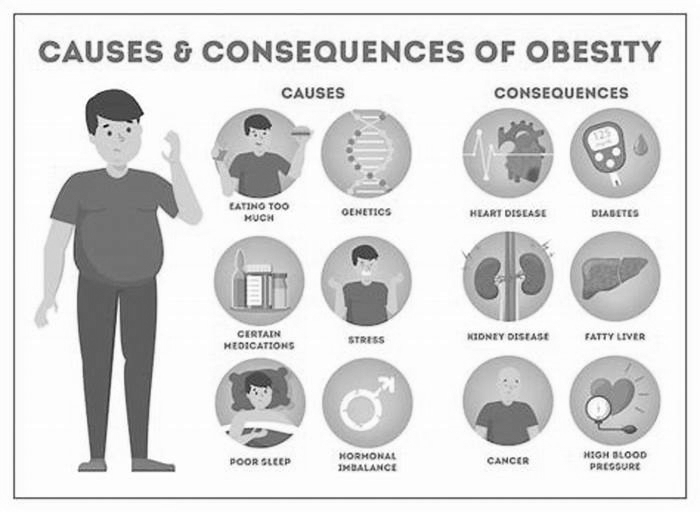
Obesity is a complex disease with many contributing factors. Neighborhood design, access to healthy, affordable foods and beverages, and access to safe and convenient places for physical activity can all impact obesity. Racial and ethnic disparities in obesity underscore the need to address social determinants of health such as poverty, education, and housing to remove barriers to health. Equitable access to obesity prevention and treatment is also needed to slow the obesity epidemic. Policy makers and community leaders can work to ensure that their communities, environments, and systems support a healthy, active lifestyle for all.
The Federal government is
- Studying what works in communities to make it easier for people to be more physically active and have a healthier diet.
- Measuring trends in obesity and related risk factors.
- Developing and promoting guidelines on dietary patternsand amounts of physical activity Americans need for good health.
- Helping families with lower incomes get affordable, nutritious foodsthrough programs such as the Supplemental Nutrition Program for Women, Infants, and Children (WIC), Pandemic Electronic Benefit Transfer, and farm-to-education programs.
- Supporting children and families who are at higher risk for obesity through services at Federally Qualified Health Centers, Head Start, WIC, and other service agencies.
- Funding programs and providing training and resources for initiatives that support breastfeeding, promote healthy eating, food and nutrition security, and physical activity.
Some states and communities are
- Making it easier to choose healthy food options where people live, work, learn, and play.
- Making healthy foods more available by connecting local producers with retailers and organizations such as childcare, schools, hospitals, and food hubs.
- Promoting nutrition standards in early care and education settings, food pantries, and faith-based organizations.
- Partnering with business and civic leaders to plan and carry-out local, culturally tailored interventions to address poor nutrition, and physical inactivity and tobacco use.
- Designing communities that connect sidewalks, bicycle routes, and public transportation with homes, early care and education settings, schools, parks, and workplaces.
Healthcare providers can
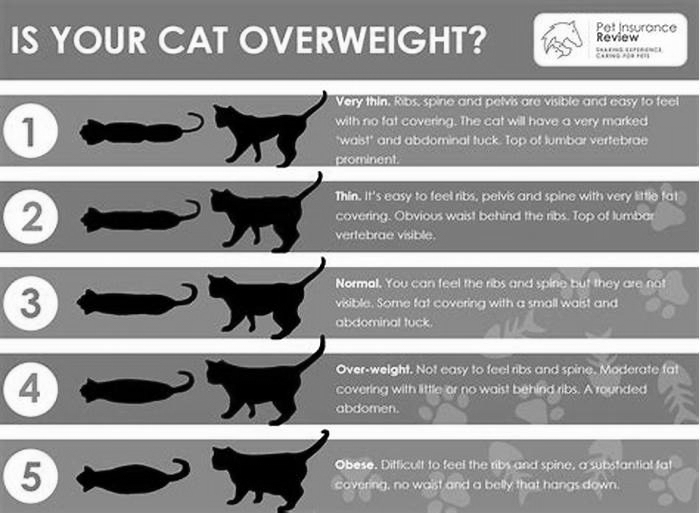
- Measure patients weight, height, and body mass index, and counsel them on keeping a healthy weight and its role in disease prevention.
- Screen children and adults for overweight and obesity and refer patients with obesity to intensive programs, including family healthy weight programs and the Diabetes Prevention Program.
- Counsel patients about nutrition, physical activity, and optimal sleep.
- Use respectful and non-stigmatizing, person-first language with all individuals in weight-related discussions.
- Connect patients and families with community services to help them have easier access to healthy food and ways to be active.
- Discuss the use of medications and other treatments for excess weight.
- Seek out continuing medical education on the latest on obesity science.
Everyone can
- Eat a healthy diet by following the 2020-2025 Dietary Guidelines for Americans.
- Get the amount of physical activity recommended by the Physical Activity Guidelines for Americans, 2nd edition.
- Get involved in community efforts to improve options for healthier foods and physical activity.
- Lose weight, if they weigh more than recommended, to help reduce risk for many chronic diseases.
- Get enough sleep.
- Manage stress.
- Talk to their healthcare providers about available obesity prevention and treatment options to help reduce potential health risks.
Solving the obesity crisis
On World Obesity Day, Dr Renata Micha outlines the scale of the worlds obesity crisis, and explains why 2021 is a crucial year for authorities if they are to solve a growing crisis.
Obesity is on the rise, and current initiatives and policies aimed at fighting it have been insufficient to reverse the trend. The success of tackling the obesity pandemic depends on governments, businesses and civil society working together to fix inadequacies in our food and health systems, focusing on better nutrition and diets for all.
This year, on World Obesity Day, it has never been more important to recognise that improving nutrition and addressing poor diets needs to be at the forefront of collective efforts to tackle obesity. The Covid-19 pandemic is interlinked with the slower, yet no less devastating, pandemic of food and nutrition insecurity, obesity, diabetes and other diet-related conditions. The top predictors of severe Covid-19 complications, other than age, are diet-related risks such as obesity, diabetes, hypertension and cardiovascular disease. In fact, a recent global analysis suggests that being obese doubles the risk of hospital treatment and increases the risk of dying from Covid-19 by nearly 50%.
Obesity is no longer just an issue in wealthier countries. Levels are on the rise in most countries, with a dramatic knock-on effect on health, quality of life, productivity, inequities and healthcare costs. According to the latest data from the Global Nutrition Report, one in three people globally are overweight or obese, while no country is on course to halt the rise of obesity. In the last two decades, the number of children categorised as overweight or obese has more than doubled on a global scale, with data showing an increase of 3.3% to 7.8% among boys aged five to 19, and 2.5% to 5.6% among girls of the same age.
Countries can no longer afford to neglect the global nutrition crisis that has led to the obesity pandemic. At least 2.8 million people around the world die each year as a result of being overweight or obese. At the same time, the global medical costs of treating the consequences of obesity are staggering and expected to rise to $1.2 trillion annually by 2025. Good nutrition is central to tackling obesity and to building healthier, more resilient populations that are better equipped against Covid-19 and future pandemics.
A shift in mindset
To stop the obesity pandemic, the world needs a shift in mindset, recognising that this is not simply a matter of individual choices but a systemic issue that governments, civil society and businesses can and should solve.
Access to healthy, affordable food depends on our food systems, which are currently contributing to poor diets, food insecurity, rising obesity levels, growing inequities and environmental pressures. Even with the unprecedented rise in diet-related diseases, in many parts of the world, agricultural production still focuses on staple commodities, rather than a broader range of more diverse, healthier foods, such as fruits, vegetables and nuts. Fresh, perishable foods are often less accessible and affordable compared to staple foods, meaning that for many, eating healthily is not a viable option. Meanwhile, junk food is widely available, cheap and intensively marketed, with advertising often targeting children and lower income communities.
Solutions that work are emerging around the world to help address food and nutrition. Governments are implementing fiscal incentives and disincentives, such as subsidies for fruits and vegetables and taxes on sugar-sweetened beverages. Regulations around point-of-purchase labelling, such as those adopted by Chile, marketing restrictions such as the UKs recent proposal to ban online junk food advertising, as well as added sugar and sodium reduction targets for the food industry released in the US, all go a long way towards promoting healthier diets and reducing diet-related diseases.
These solutions now need to be scaled up dramatically, along with new evidence-based policies that go beyond educational policy measures to transform food systems and address obesity. This will require mobilisation from the academic community to prioritise research on innovative food and nutrition strategies. Crucially, it requires concerted action and investments from governments, businesses and civil society, working across sectors, to implement food and nutrition priorities that benefit all.
Better integration of nutrition into healthcare systems is also critical. Even before Covid-19, healthcare systems were overwhelmed by diet-related diseases. Yet, in many parts of the world, nutrition care is entirely absent from healthcare systems. Nutrition care needs to be made universally available, given the role it plays in determining our health and wellbeing.
A year for action
With key moments including the UN Food Systems Summit and the Tokyo Nutrition For Growth Summit on the horizon, 2021 provides a unique opportunity for governments, civil society and the private sector to work together to tackle food and nutrition through strong and measurable commitments.
This will require acting at every step of the food and nutrition chain from the way we produce and market food, to the way we help individuals adapt behaviours, make healthier choices and improve their health. Governments, civil society and the private sector will need to recognise the role they can play in this process and will be expected to make the bold commitments that nutrition deserves.
Renata Micha is Chair of the Independent Expert Group of the Global Nutrition Report and Associate Professor in Human Nutrition at the University of Thessaly, Greece. This blog was originally published as an op-ed in the New Food Magazine.
Tackling obesity is a shared responsibility for society
As Health Secretary, theres some guiding principles I try to follow, like: always start with the patients, follow the evidence, listen to the experts, and then make decisions that do the most good not the ones that are most politically expedient.
Although, as President Roosevelt once said: Theres as many opinions as there are experts.
So its great to be here with so many experts today, to discuss the modern challenge of obesity.
I want to start by paying tribute to the work of this APPG, who have done so much to raise the issue, and stand testament to the fact obesity is one of the biggest health challenges we face as a society. Here in Britain, and across the world.
Now, for the first time, obesity is thought to be a bigger problem, globally, than hunger.
Of course, the growing availability of food around the world is a good thing, and is something humanity has sought to achieve throughout history. But abundance of food brings new challenges.
After all, as humans we are predisposed to eat more than we need, as our evolution has designed us to stock up in abundance for leaner times ahead.
Each and every one of us, in rich nations, faces this clash of evolutionary biology and modern life every day. And its worth noting that as nations grow richer, its the poorest in them who are the most prone to obesity.
So tackling obesity means tackling social, environmental, physical and psychological pressures, and giving people the capability they need to eat healthily.
And the evidence shows that for a whole host of reasons, some people are more susceptible to obesity than others.
The question I want to address today, and which this APPG is rightly considering, is how to address obesity, and what is the role for government, for business, for civil society and for each of us as citizens. Because tackling obesity is a shared responsibility for society.
This government has taken a global lead in our obesity strategy, chapters 1 and 2, with our ambitious targets to halve childhood obesity by 2030. Our strategy sets out the scale of the problem, and also what were doing to tackle it.
Were cutting sugar in soft drinks. The sugar levy has removed the equivalent of 90 million kilograms of sugar since it was introduced in 2016, proving that population-wide measures work, and are necessary, alongside promoting healthier behaviours and empowering individuals to make better choices.
Were tackling everything from reformulation of foods, to calorie labelling in restaurants, to restricting advertising and promotion of junk food, to encouraging schools to adopt a daily mile so children are more active.
Were doubling the NHS Diabetes Prevention Programme over the next 5 years, supporting low-calorie diets for obese people with type 2 diabetes.
Just this weekend we announced our latest measures, to curb retailers fuelling promotion of unhealthy foods.
On top of our obesity strategy, our Long Term Plan for the NHS sets out how were driving the obesity strategy across the health service.
GPs are making every contact count in identifying and supporting overweight children and adults manage their weight.
Hospitals will increasingly support patients whose obesity leaves them hospitalised, with a huge burden of cost on the NHS.
Well learn from anywhere, so weve studied the success of cities like Amsterdam and their whole systems approach to reducing childhood obesity. And I want us to keep learning from the latest evidence and new approaches from around the world.
The only way were going to solve the growing, global challenge of obesity is if everyone plays their part.
The state has a vital role to play in reducing the environmental factors that contribute to obesity and protecting vulnerable children. We will play our part.
Local government has an important role supporting healthier high streets through better planning decisions, through their role in education, providing equipment for exercise, helping protect and create more open spaces for children to play and be active.
The health service itself has a vital and growing role to play in preventing obesity and helping people achieve a healthy weight.
Public Health England are world leaders in gathering and analysing data so we can make the correct, evidence-led, decisions.
Thanks to their work on identifying the role of sugar in obesity, we corrected the decades old mistake of focusing too much on saturated fat.
They will have a crucial role to play in developing the next phase of data-driven public health programmes using predictive prevention.
Companies large and small have a role to play in reformulating their products. I welcome action thats been taken so far, Im excited by some of the coming science, and I want to see more action by the food industry.
Civil society has a role to play too in supporting people to stay healthy. I want to pay tribute to individuals with big voices like Hugh Fearnley-Whittingstall and Jamie Oliver, who use their influence to try to change habits, norms and assumptions, as well as trying to change government policy. Because changing behaviour means changing norms, as well as the formal rules we set in this building.
Finally, each of us, as individuals, we have a role to play and must take responsibility for our own health. Because even with the best efforts of the state and society, we cant solve the obesity challenge without individuals taking personal responsibility too: this is a shared responsibility.
Were putting in a record 20.5 billion extra a year into the NHS the longest and largest cash settlement in its history as we transform the health service over the next decade.
To rise to the challenges of today and seize the opportunities of the future, were implementing the new NHS Long Term Plan on the principle that prevention is better than cure.
Its better for people if we prevent them becoming patients in the first place. Its better for the NHS if they help people stay healthy rather than treating them only when they fall ill. And its better for taxpayers, and the nation, if we build a sustainable health system that will be there, for all of us, in years to come. The prevention agenda means yes, making changes only government can make.
That same prevention agenda means we need to do more to support people to take care of themselves, to keep themselves healthy to empower people with the capability and expectation that they have an important role to play too.
I want to take a moment to set out the approach I take to these sorts of interventions.
I am no fan of nanny state interventions that treat everyone the same, or punish the masses for the problems of a minority.
The blanket public health approach we needed in an age of contagious diseases is still needed now in some areas. But the modern public health problems of largely non-communicable diseases need a different attitude, and a much more targeted approach.
No organisation wanting to tackle a problem as big as obesity would use the same approach for everyone, and target the whole population the same. After all, food is safe, obviously critical, as part of a balanced diet. Even a fatty cut of delicious steak is healthy in moderation.
There is huge, overwhelming, support for action to tackle obesity. Lets not lose that support with too much of a blanket approach.
Take alcohol. For 95% of people, the alcohol we drink is perfectly safe and normal. I like a pint or the odd glass of wine, and I know I speak for most of my audience and certainly the vast majority of my colleagues too. Lets not punish the masses for perfectly healthy behaviour.
But for the 5% who drink around a third of all the alcohol consumed, who too often end up hospitalised and seriously ill because of it, we need much more serious intervention.
The same attitude is needed across public health: lots more targeting, less intervention for the healthy, more intervention for those who need it. And the exciting thing is, we have a radically expanding toolkit at our disposal.
The approach we take with a 60-year-old man, whos set in his ways, must be different to the approach we take with a young, pregnant mother trying to get healthy for the sake of her baby.
And in the future, as we unlock our genetic codes and adopt new technologies like artificial intelligence, we can be yet more targeted too. We can even get ahead of the problem, supporting people who are likely to have problems with help and nutritional support.
With the right attitude and technology, we can lead the world with predictive prevention and personalised health services.
This approach can only work if we see tackling obesity as a shared responsibility. Diet and physical activity too much and too little are, by far and away, the 2 biggest factors that contribute to obesity. And the best solutions are in the vast majority of cases not medicinal, but behavioural.
The role of the health service is just as much to prescribe behaviour change as it is to prescribe drugs. This is now widely accepted, but needs to be embedded in the way we organise our NHS.
Nutritional advice, counselling, activity and exercise must be just as much a part of the toolkit of the NHS as drugs. This insight is behind our strong support for social prescribing, embedded in our NHS Long Term Plan.
This agenda is so important were going to introduce more than 1,000 trained social prescribing link workers within the next 2 years, to help refer over 900,000 people because the evidence shows that social prescribing, like activity or an exercise classes, can lead to the same or better outcomes than drugs.
I also strongly believe that because many of those social cures are free, they dont have multi-million dollar marketing budgets behind them. So its the job of those of us in government to compensate and lean in supporting training and developing the evidence base for social prescribing.
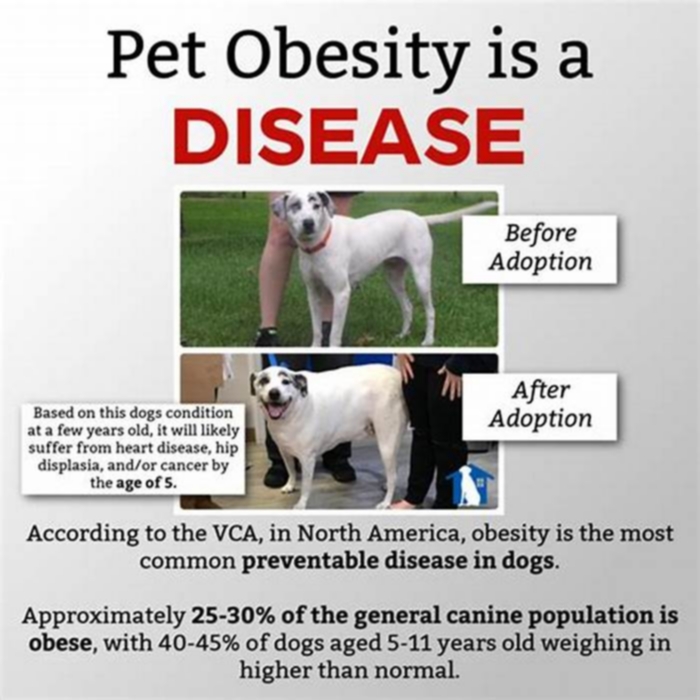
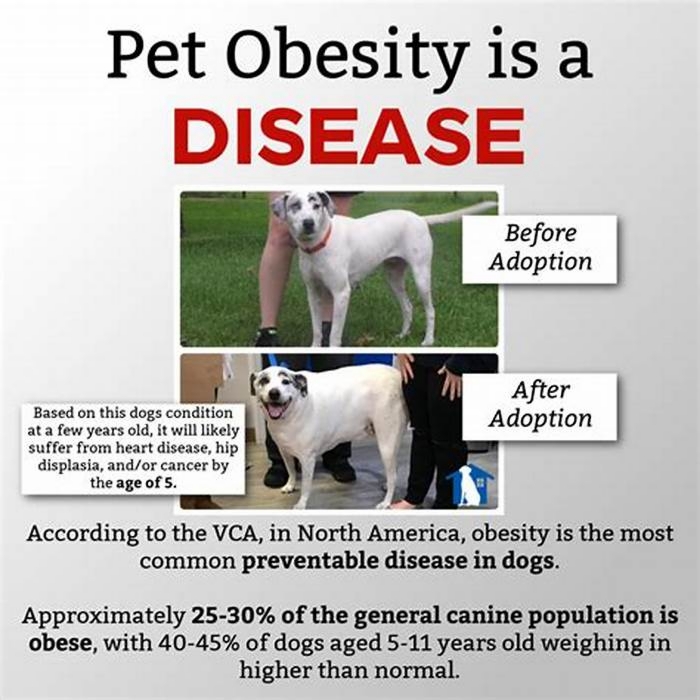
And that brings me to the definitional issue. I understand the reasons why some have called for obesity to be reclassified as a disease. People rightly want to lessen the stigma and increase support for people with obesity.
I agree with both of those goals. Ive listened to the various views within the medical system, and Ive taken advice. And Im a staunch supporter of action to tackle obesity.
But I think reclassifying obesity isnt the way to do it. In trying to reduce one stigma, we risk creating another. I worry that calling obesity a disease, like cancer, risks being counter-productive and sending out the wrong message.
And because obesity is a condition born of human behaviour, my biggest worry is that if people with obesity are told they have a disease, it risks robbing them of agency and the incentive to change behaviour.
We risk taking away their power, where we must do everything we can to support and empower and expect them to change their lives through healthier choices.
Instead of helping them, we make them feel helpless. I dont think that helps. Is that what we want? More drugs and medical solutions encouraging life-long dependency on prescriptions and pills? No: we should have high expectations and support people to meet them.
Now, I know theres a healthy debate around this, and I welcome todays event and a frank and public discussion, because anything we can do to increase the focus on and reduce the stigma around obesity is hugely welcome. We share the same goal: to reduce obesity and help people live healthier lives.
But, while we shouldnt call obesity a disease, we should redouble our efforts to act. And perhaps nowhere is the prevention agenda more important than childhood obesity.
Almost a quarter of 4 and 5 year-olds are now overweight or obese, and that rises to a third by the time children are 11.
We must prevent overweight kids from becoming obese adults. And for children, I do believe in the strongest government interventions.
Lets help families and empower parents to lead healthier and more active lives, for the sake of the children. Lets make Britain the best place for children to grow up, where a childs health and life chances arent curtailed by obesity before they even start secondary school. Lets treat healthy adults like healthy adults, and treat children like children.
Prevention will be embedded into every part of the NHS over the next decade. State, society, business and people. We each have our part to play.
We have a shared responsibility to work together to tackle obesity and build the health system and society we all want to see.