What are examples of secondary prevention
Bookshelf
Definition/Introduction
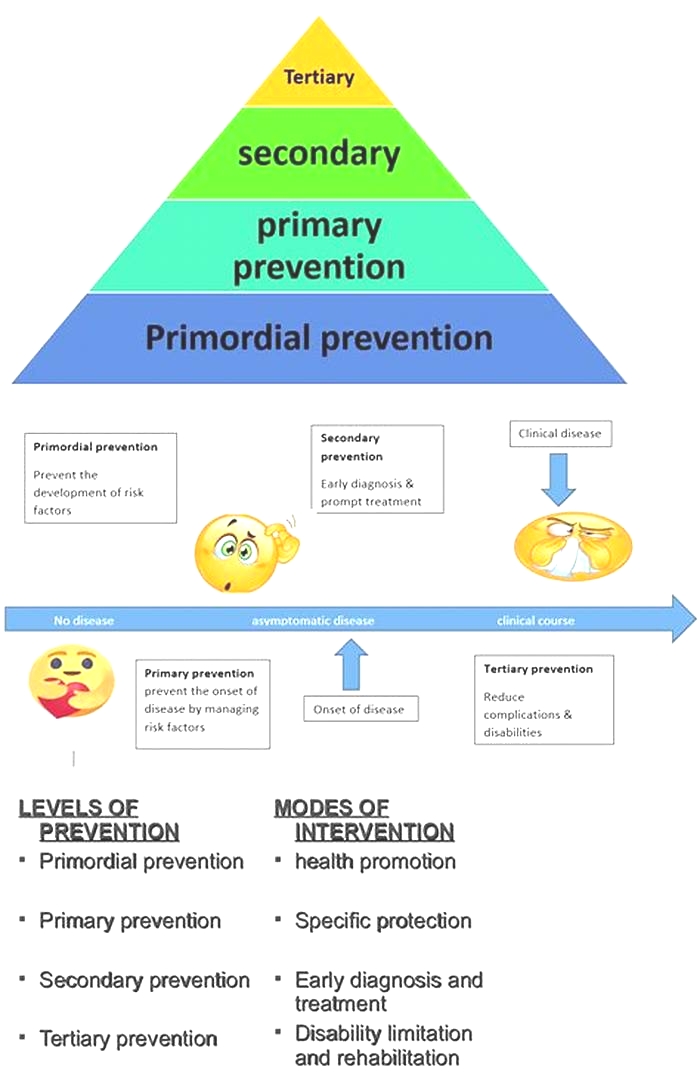
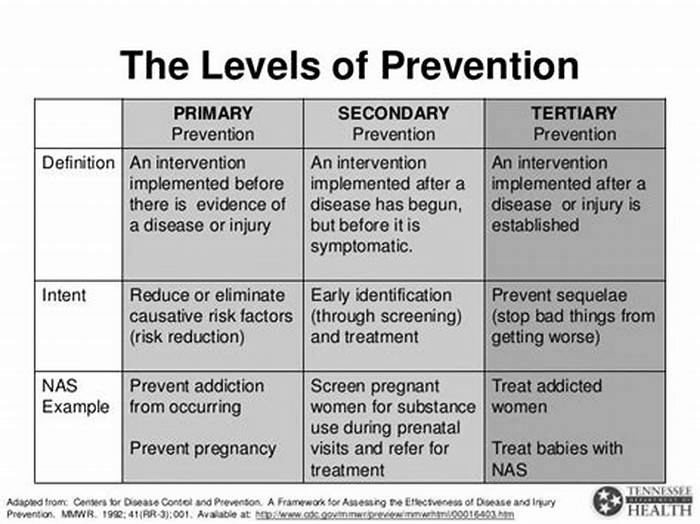
The natural history of a disease classifies into five stages: underlying, susceptible, subclinical, clinical, and recovery/disability/death. Corresponding preventive health measures have been grouped into similar stages to target the prevention of thesestages of a disease. These preventive stages are primordial prevention, primary prevention, secondary prevention, and tertiary prevention. Combined, these strategies not only aim to prevent the onset of disease through risk reduction but also downstream complications of a manifested disease.
Primordial Prevention
In 1978, the most recent addition to preventive strategies, primordial prevention, was described. It consists of risk factor reduction targeted towards an entire population through a focus on social and environmental conditions. Such measures typically get promoted through laws and national policy. Because primordial prevention is the earliest prevention modality, it is often aimed at children to decrease as much risk exposure as possible. Primordial prevention targets the underlying stage of natural disease by targeting the underlying social conditions that promote disease onset. An example includes improving access to an urban neighborhood to safe sidewalks to promote physical activity; this, in turn, decreases risk factors for obesity, cardiovascular disease, type 2 diabetes, etc.
Primary Prevention
Primary prevention consists of measures aimed at a susceptible population or individual. The purpose of primary prevention is to prevent a disease from ever occurring. Thus, its target population is healthy individuals. It commonly institutes activities that limit risk exposure or increase the immunity of individuals at risk to prevent a disease from progressing in a susceptible individual to subclinical disease. For example, immunizations are a form of primary prevention.
Secondary Prevention
Secondary prevention emphasizes early disease detection, and its target is healthy-appearing individuals with subclinical forms of the disease. The subclinical disease consists of pathologic changes but no overt symptoms that are diagnosable in a doctor's visit. Secondary prevention often occurs in the form of screenings. For example, a Papanicolaou (Pap) smear is a form of secondary prevention aimed to diagnose cervical cancer in its subclinical state before progression.
Tertiary Prevention
Tertiary prevention targets both the clinical and outcome stages of a disease. It is implemented in symptomatic patients and aims to reduce the severity of the disease as well as any associated sequelae. While secondary prevention seeks to prevent the onset of illness, tertiary prevention aims to reduce the effects of the disease once established in an individual. Forms of tertiary prevention are commonly rehabilitation efforts.
Quaternary Prevention
According to the Wonca International Dictionary for General/Family Practice, quaternary prevention is "action taken to identify patients at risk of overmedicalization, to protect him from new medical invasion, and to suggest to him interventions, which are ethically acceptable." Marc Jamoulle initially proposed this concept, and the targets were mainly patients with illness but without the disease. The definition has undergone recent modification as "an action taken to protect individuals (persons/patients) from medical interventions that are likely to cause more harm than good." [1]
Issues of Concern
In the United States, several governing bodies make prevention recommendations. For example, the United States Preventive Services Task Force (USPSTF) is a governing body that makes recommendations for primary and secondary prevention strategies. The Advisory Committee on Immunizations Practices (ACIP) through the Centers for Disease Control and Prevention (CDC) makes recommendations for vaccinations, while the Womens Preventive Services Initiative (WPSI) makes recommendations appropriate for females. Additionally, various specialty organizations, such as the American College of Obstetrics and Gynecology (ACOG) and the American Cancer Society (ACS), etc. also make prevention recommendations. With the multitude of information and recommending bodies, it is often challenging for healthcare professionals to remain up to date on changing endorsements.
Further, while preventive services are regulated and must undergo scrutinous safety testing, there is risk involved with prevention. Particularly primary and secondary preventive factors targeted at intervening in healthy-appearing individuals. It is often challenging to gain buy-in from patients regarding the risk-benefit ratio of various preventive services.
Finally, the cost of preventive services is commonly a topic of discussion. Several cost-benefit analyses have been undertaken regarding the evaluation of preventive services with varying degrees of confidence. While often a long-term gain of healthy life years is noted, preventive services are not inexpensive, which can limit the use of these services by both healthcare systems and patients and is a consideration when promoting preventive services.
Clinical Significance
Preventive services have proven an essential aspect of healthcare; however, they appear consistently underutilized in the United States.[2][3][4] With cost, time, and resource constraints on physicians, many preventive services get overlooked. Physicians need to remain up to date on the prevention guidelines and ensure all patients are offered appropriate services with a full explanation of risks and benefits.
Some examples of commonly used prevention strategies are:
Primordial
Primary
Secondary
Tertiary
Quarternary
The following conditions are susceptible to over-treatment:
Radiological incidentalomas
[9]The use of antiarrhythmic drugs after myocardial infarction that reduced arrhythmias but increased mortality
The use of hormone replacement therapy led to an increased number of cases of breast cancer, stroke, and thromboembolic events. It was also a failure in reducing cardiovascular mortality.
Medically unexplained symptoms
Functional disorders
Bodily distress syndrome
[10]
Nursing, Allied Health, and Interprofessional Team Interventions
Proper communication among the various healthcare personnel should be there to provide appropriate levels of prevention to the general public and patients. School staff and other ancillary staff require education on the importance of providing prevention as an important aspect of caring for an individual while he/she is a student.
Cookies on the NHS England website
High impact interventions for the prevention and treatment of cardiovascular disease, diabetes and respiratory disease
There is a strong rationale for Integrated Care Systems (ICSs) and their partners to prioritise prevention. Over the last century we have seen significant improvements in healthy life expectancy driven, in part, by improvements in secondary prevention. Since, 2010 however, these improvements have stalled; particularly amongst more deprived communities, further exacerbating health inequalities, which are driven by a higher prevalence of modifiable risk factors within certain population groups, particularly the Core20PLUS5 population.
The DHSC has reported non-Covid excess mortality since July 2021, primarily driven by cardiovascular disease (CVD), liver disease, and diabetes. In addition, the NHS is experiencing a sustained period of high demand for urgent and emergency care, with analysis showing respiratory disease and CVD (for which diabetes is a major risk factor), amongst the leading drivers of A&E admissions.
There is extensive evidence on prevention interventions which work and deliver rapid improvements. For example, regular diagnosis and treatment of high blood pressure, atrial fibrillation or abnormal heart rate and high cholesterol to prevent progression of CVD has a significant, rapid and tangible impact on the health of the population (alongside population-level preventative interventions, such as cancer screening programmes).
A return to delivery at pre-pandemic levels, whilst extending the reach of existing services to address health inequalities, is crucial. We must ensure effective interventions reach populations which dont traditionally engage with these services. Its in these groups where the greatest impact can be made with ICSs providing an excellent opportunity to rethink how prevention interventions are systematically delivered, to achieve a real shift in outcomes across the population.
To support the development of prevention strategies by ICSs, NHS England in partnership with NICE, have developed the resource below: setting out advice on the most impactful interventions relating to the prevention and management of CVD, diabetes and respiratory disease. There is a robust evidence base for them, which should deliver benefits at an individual patient level, based on a summary of the existing evidence and resources available.
Modifiable Risk Factors
- Tobacco dependence identification and treatment in secondary care
- Weight management services for people with diabetes and/or hypertension
- Alcohol care teams.
View as a pdf or view as accessible web pages
Respiratory
- Spirometry in diagnosis of asthma and chronic obstructive pulmonary disease (COPD)
- Inhaler and medicines optimisation
- Pulmonary rehabilitation for COPD
- Personalised asthma action plan for all children and young people with asthma.
View as a pdf or view as accessible web pages
Diabetes
- Structured education
- NHS Diabetes Prevention programme
- Delivery of 9 diabetes care processes.
View as a pdf or view as accessible web pages
CVD
- Community pharmacy hypertension case finding
- Cholesterol search and risk stratification
- NHS health check
- Case finding and direct-acting oral anticoagulation to prevent atrial fibrillation related strokes
- Cardiac rehabilitation for patients post-ACS and diagnosis of heart failure
- Optimisation of hypertension treatment
- Optimisation of heart failure treatment through annual reviews
- Optimising management post ACS, including lipid management.
View as a pdf or view as accessible web pages
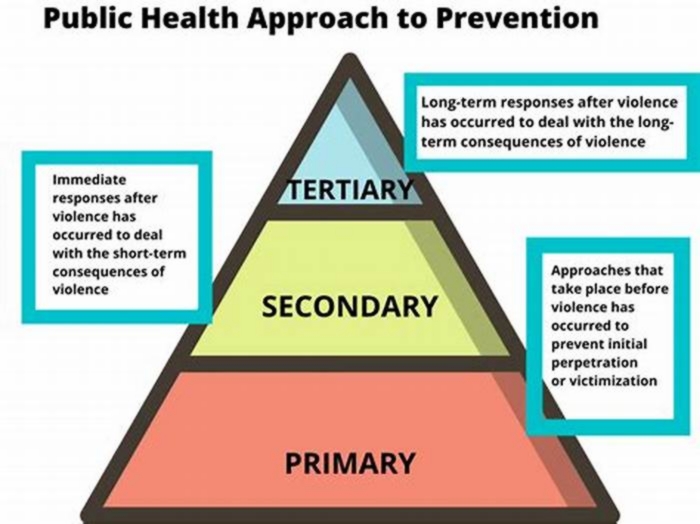
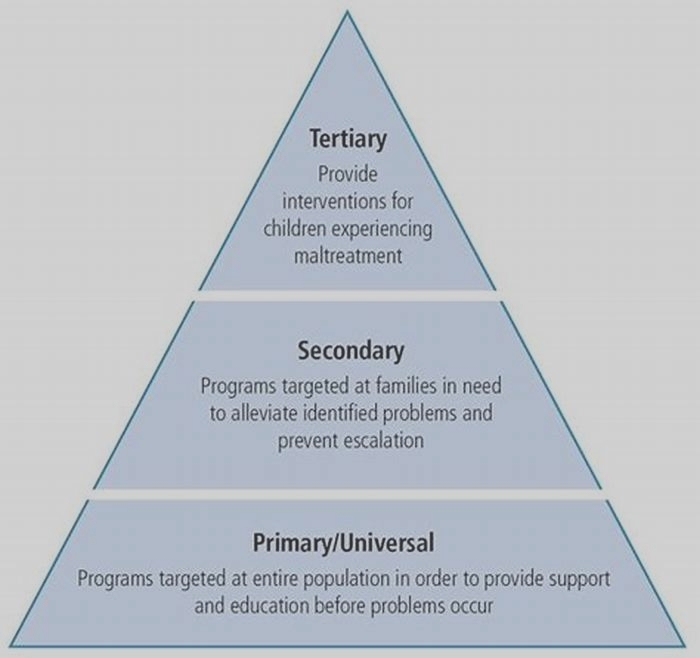
Primary, secondary and tertiary prevention
Prevention includes a wide range of activities known as interventions aimed at reducing risks or threats to health. You may have heard researchers and health experts talk about three categories of prevention: primary, secondary and tertiary. What do they mean by these terms?
Primary prevention
Primary preventionaims to prevent disease or injury before it ever occurs. This is done by preventing exposures to hazards that cause disease or injury, altering unhealthy or unsafe behaviours that can lead to disease or injury, and increasing resistance to disease or injury should exposure occur. Examples include:
- legislation and enforcement to ban or control the use of hazardous products (e.g. asbestos) or to mandate safe and healthy practices (e.g. use of seatbelts and bike helmets)
- education about healthy and safe habits (e.g. eating well, exercising regularly, not smoking)
- immunization against infectious diseases.
Secondary prevention
Secondary preventionaims to reduce the impact of a disease or injury that has already occurred. This is done by detecting and treating disease or injury as soon as possible to halt or slow its progress, encouraging personal strategies to prevent reinjury or recurrence, and implementing programs to return people to their original health and function to prevent long-term problems. Examples include:
- regular exams and screening tests to detect disease in its earliest stages (e.g. mammograms to detect breast cancer)
- daily, low-dose aspirins and/or diet and exercise programs to prevent further heart attacks or strokes
- suitably modified work so injured or ill workers can return safely to their jobs.
Tertiary prevention
Tertiary preventionaims to soften the impact of an ongoing illness or injury that has lasting effects. This is done by helping people manage long-term, often-complex health problems and injuries (e.g. chronic diseases, permanent impairments) in order to improve as much as possible their ability to function, their quality of life and their life expectancy. Examples include:
- cardiac or stroke rehabilitation programs, chronic disease management programs (e.g. for diabetes, arthritis, depression, etc.)
- support groups that allow members to share strategies for living well
- vocational rehabilitation programs to retrain workers for new jobs when they have recovered as much as possible.
Going upstream
To help explain the difference, take this example. Lets say you are the mayor of a town near a swimming hole used by kids and adults alike. One summer, you learn that citizens are developing serious and persistent rashes after swimming as a result of a chemical irritant in the river. You decide to take action.
If you approach the company upstream that is discharging the chemical into the river and make it stop, you are engaging in primary prevention. You are removing the hazardous exposure and preventing rashes in the first place.
If you ask lifeguards to check swimmers as they get out of the river to look for signs of a rash that can then be treated right away, you are engaging in secondary prevention. You are not preventing rashes, but you are reducing their impact by treating them early on so swimmers can regain their health and go about their everyday lives as soon as possible.
If you set up programs and support groups that teach people how to live with their persistent rashes, you are engaging in tertiary prevention. You are not preventing rashes or dealing with them right away, but you are softening their impact by helping people live with their rashes as best as possible.
For many health problems, a combination of primary, secondary and tertiary interventions are needed to achieve a meaningful degree of prevention and protection. However, as this example shows, prevention experts say that the further upstream one is from a negative health outcome, the likelier it is that any intervention will be effective.
Source:At Work, Issue 80, Spring 2015: Institute for Work & Health, Toronto [This column updates a previous column describing the same term, originally published in 2006.]