What are 5 examples of primary prevention
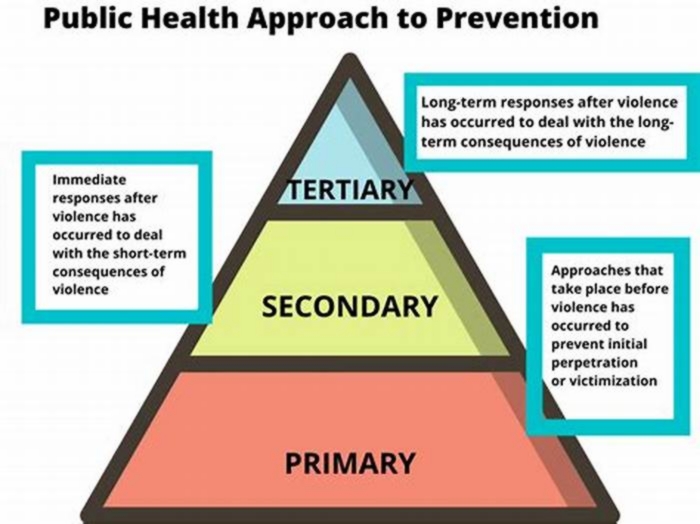
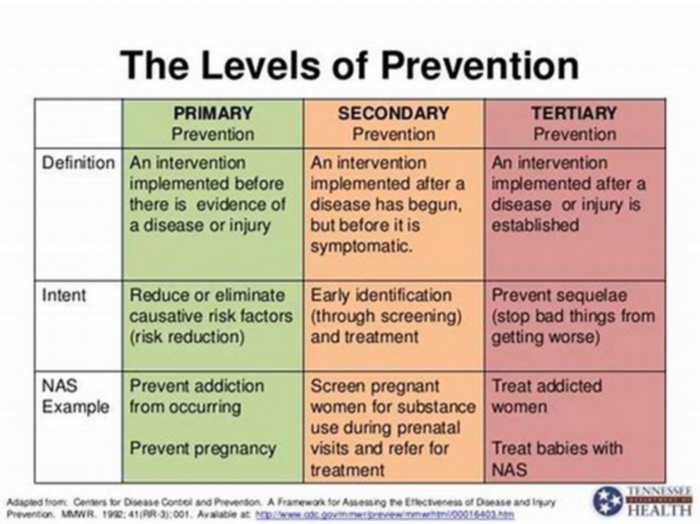
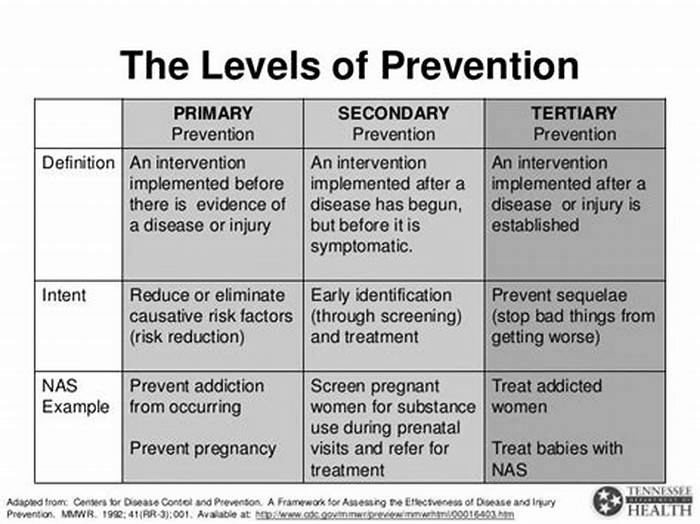
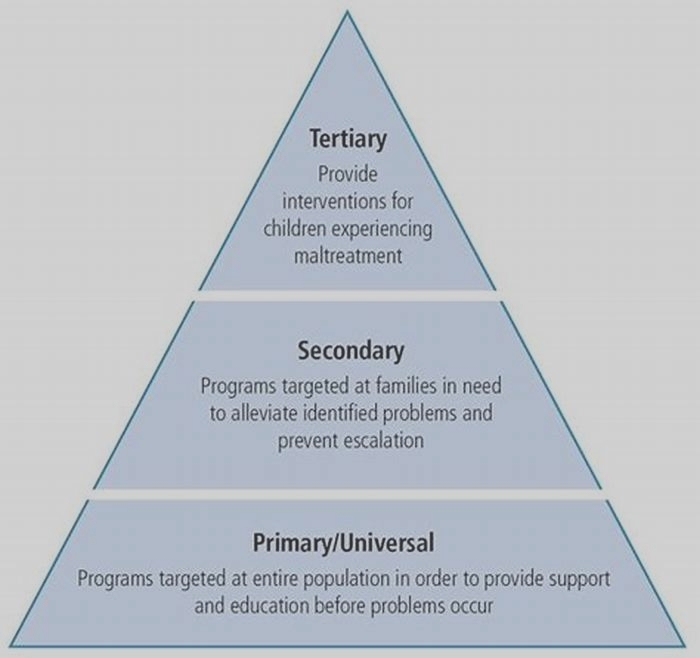
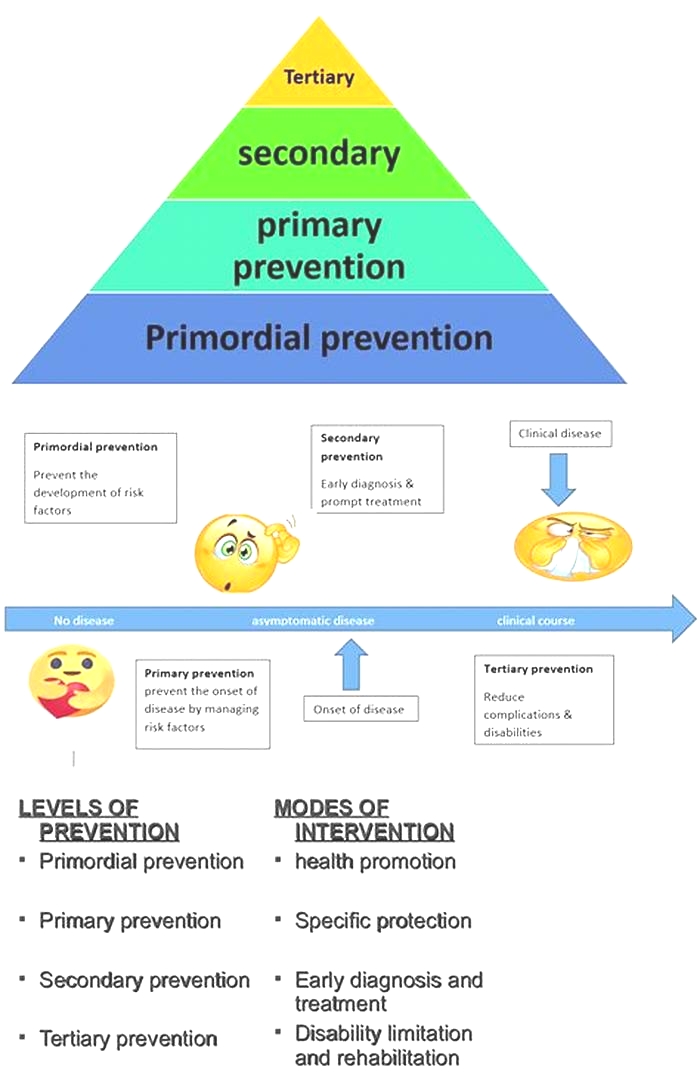
The three levels of prevention are primary, secondary, and tertiary.
In primary prevention, a disorder is actually prevented from developing.
Types of primary prevention include the following:
In secondary prevention, disease is detected and treated early, often before symptoms are present, thus minimizing serious consequences.
Types of secondary prevention include the following:
Screening programs, such as mammography to detect breast cancer and dual x-ray absorptiometry (DXA) to detect osteoporosis.
Tracking down the sex partners of a person diagnosed with a sexually transmitted infection (contact tracing) and, if necessary, treating these people to minimize spread of the disease.
In tertiary prevention, an existing, usually chronic disease is managed to prevent complications or further damage.
Types of tertiary prevention include the following:
For people with diabetes: Control of blood sugar, excellent skin care, frequent examination of the feet, and frequent exercise to prevent heart and blood vessel disorders
Providing supportive and rehabilitative services to prevent deterioration and maximize quality of life, such as rehabilitation from injuries, heart attack, or stroke
Preventing complications in people with disabilities, such as preventing pressure sores in those confined to bed.
2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary
Circulation. Author manuscript; available in PMC 2021 Aug 9.
Published in final edited form as:
PMCID: PMC8351755
NIHMSID: NIHMS1722052
2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary
A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines
, PhD, MSPH, FAHA, Co-Chair, , MD, FACC, FAHA, Co-Chair, , MD, MPH, FAHA,* , MD, MHS, FACC, FAHA,* , Esq, , MD, MPH,* , MD, MS, FACC, FAHA, , MD, MPA, FACC,* , PhD, RN,* , MD, MACC, FAHA,* , PhD, RN, ANP, FAHA,* , MD, PhD, FACC, FAHA,* , MD, MSc, FACC, FAHA,* , MD, MACC, FAHA,* , MD, SCM, FACC, FAHA,* , MD, MS, FACC, FAHA,* , MBBCh, MEd, MHS,* and , MD, PhD, FACC, FAHA
Donna K. Arnett
University of Kentucky College of Public HealthDean and Professor of Epidemiology
Roger S. Blumenthal
Johns Hopkins UniversityProfessor of Medicine and Director, Ciccarone Center for the Prevention of Heart Disease
Michelle A. Albert
UCSF School of MedicineProfessor of Medicine and Director, UCSF NURTURE Center
Erin D. Michos
Johns Hopkins School of MedicineAssociate Professor of Medicine and Associate Director of Preventive Cardiology, Ciccarone Center for the Prevention of Heart Disease; Johns Hopkins Bloomberg School of Public HealthAssociate Professor of Epidemiology
Andrew B. Buroker
Faegre Baker Daniels LLP, Partner
Michael D. Miedema
Minneapolis Heart InstituteDirector of Cardiovascular Prevention
Zachary D. Goldberger
University of Wisconsin School of Medicine and Public HealthAssociate Professor of Medicine, Division of Cardiology
Daniel Muoz
Vanderbilt University Medical CenterAssistant Professor of Medicine, Division of Cardiology, Medical Director for Quality, Vanderbilt Heart & Vascular Institute, and Associate Medical Director, Cardiovascular ICU
Ellen J. Hahn
University of Kentucky College of NursingProfessor & Director, BREATHE, Deputy Director, UKCARES & Leader, and Community Engagement Core; Marcia A. Dake Professor of Nursing
Sidney C. Smith, Jr
University of North Carolina, Chapel HillProfessor of Medicine, Division of Cardiology
Cheryl D. Himmelfarb
Johns Hopkins School of NursingProfessor; Associate Dean Research, Office for Science and Innovation; and Deputy Director, Johns Hopkins Institute for Clinical and Translational Research
Salim S. Virani
Baylor College of MedicineProfessor, Section of Cardiovascular Research and Director for Research, Cardiology Fellowship Training Program; Michael E. DeBakey VA Medical CenterStaff Cardiologist and Investigator, Health Policy, Quality & Informatics Program, Center for Innovations in Quality, Effectiveness and Safety
Amit Khera
UT Southwestern School of MedicineProfessor of Internal Medicine and Director, Preventive Cardiology Program
Kim A. Williams, Sr
Rush Medical CollegeJames B. Herrick Professor and Chief, Division of Cardiology, Department of Internal Medicine
Donald Lloyd-Jones
Northwestern UniversityEileen M. Foell Professor; Senior Associate Dean for Clinical and Translational Research; Chair, Department of Preventive Medicine; and Director, Clinical and Translational Sciences Institute
Joseph Yeboah
Wake Forest Baptist HealthAssociate Professor, Internal Medicine, Cardiovascular
J. William McEvoy
National University of Ireland, Galway CampusProfessor of Preventive Cardiology; National Institute for Preventive Cardiology, GalwayMedical and Research Director; and University Hospital Galway, IrelandConsultant Cardiologist.
Boback Ziaeian
University of California at Los Angeles, David Geffen School of MedicineClinical Instructor, Division of Cardiology
Donna K. Arnett, University of Kentucky College of Public HealthDean and Professor of Epidemiology;
Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Geriatrics Society, the American Society of Preventive Cardiology, and the Preventive Cardiovascular Nurses Association
*ACC/AHA Representative.
Lay Representative.
ACC/AHA Task Force on Clinical Practice Guidelines Liaison.
Task Force Performance Measures Representative.
Former Task Force member; current member during the writing effort.
Presidents and Staff
American College of Cardiology
C. Michael Valentine, MD, FACC, President
Timothy W. Attebery, MBA, FACHE, Chief Executive Officer
William J. Oetgen, MD, MBA, FACC, Executive Vice President, Science, Education, Quality, and Publishing
MaryAnne Elma, MPH, Senior Director, Science, Education, Quality, and Publishing
Amelia Scholtz, PhD, Publications Manager, Science, Education, Quality, and Publishing
American College of Cardiology/American Heart Association
Katherine A. Sheehan, PhD, Director, Guideline Strategy and Operations
Abdul R. Abdullah, MD, Senior Manager, Guideline Science
Thomas S.D. Getchius, Manager, Guideline Operations
American Heart Association
Ivor Benjamin, MD, FAHA, President
Nancy Brown, Chief Executive Officer
Rose Marie Robertson, MD, FAHA, Chief Science and Medicine Officer
Gayle R. Whitman, PhD, RN, FAHA, FAAN, Senior Vice President, Office of Science Operations
Cammie Marti, PhD, MPH, RN, Science and Medicine Advisor, Office of Science Operations
Jody Hundley, Production and Operations Manager, Scientific Publications, Office of Science Operations
The publisher's final edited version of this article is available free at
Circulation- Supplementary Materials
targeted literature searches.
GUID:6DFB14AF-58D7-4B6E-A9D6-A5E11BF625AC
web supplement.
GUID:F87B49F5-3E41-4679-BEE8-B0344D7EE275
comprehensive relationships table.
GUID:6B2FB945-98A0-4C58-8AAB-5E78403357F1
data supplement.
GUID:6D719DBB-226B-40D8-93A1-426F3869CE8A
Top 10 Take-Home Messages for the Primary Prevention of Cardiovascular Disease
1. The most important way to prevent atherosclerotic vascular disease, heart failure, and atrial fibrillation is to promote a healthy lifestyle throughout life.
2. A team-based care approach is an effective strategy for the prevention of cardiovascular disease. Clinicians should evaluate the social determinants of health that affect individuals to inform treatment decisions.
3. Adults who are 40 to 75 years of age and are being evaluated for cardiovascular disease prevention should undergo 10-year atherosclerotic cardiovascular disease (ASCVD) risk estimation and have a clinicianpatient risk discussion before starting on pharmacological therapy, such as antihypertensive therapy, a statin, or aspirin. The presence or absence of additional risk-enhancing factors can help guide decisions about preventive interventions in select individuals, as can coronary artery calcium scanning.
4. All adults should consume a healthy diet that emphasizes the intake of vegetables, fruits, nuts, whole grains, lean vegetable or animal protein, and fish and minimizes the intake of trans fats, processed meats, refined carbohydrates, and sweetened beverages. For adults with overweight and obesity, counseling and caloric restriction are recommended for achieving and maintaining weight loss.
5. Adults should engage in at least 150 minutes per week of accumulated moderate-intensity physical activity or 75 minutes per week of vigorous-intensity physical activity.
6. For adults with type 2 diabetes mellitus, lifestyle changes, such as improving dietary habits and achieving exercise recommendations are crucial. If medication is indicated, metformin is first-line therapy, followed by consideration of a sodium-glucose cotransporter 2 inhibitor or a glucagon-like peptide-1 receptor agonist.
7. All adults should be assessed at every healthcare visit for tobacco use, and those who use tobacco should be assisted and strongly advised to quit.
8. Aspirin should be used infrequently in the routine primary prevention of ASCVD because of lack of net benefit.
9. Statin therapy is first-line treatment for primary prevention of ASCVD in patients with elevated low-density lipoprotein cholesterol levels (190 mg/dL), those with diabetes mellitus, who are 40 to 75 years of age, and those determined to be at sufficient ASCVD risk after a clinicianpatient risk discussion.
10. Nonpharmacological interventions are recommended for all adults with elevated blood pressure or hypertension. For those requiring pharmacological therapy, the target blood pressure should generally be <130/80 mm Hg.
Keywords: ACC/AHA Clinical Practice Guidelines, guidelines, antihypertensive agents, aspirin, atherosclerosis, atherosclerotic cardiovascular disease, atrial fibrillation, behavior modification, behavior therapy, blood cholesterol, blood pressure, body mass, index, cardiovascular team-based care, cardiovascular, cardiovascular disease, cholesterol, chronic kidney disease, coronary artery calcium score, coronary disease, coronary heart disease, cost, diet, dietary patterns, dietary fats, dietary sodium, dyslipidemia, e-cigarettes, exercise, healthcare disparities, health services accessibility, heart failure, hypertension, LDL-cholesterol, diabetes mellitus, lifestyle, lipids, measurement, myocardial infarction, nicotine, nonpharmacological treatment, nutrition, physical activity, prejudice, primary prevention, psychosocial deprivation, public health, quality indicators, quality measurement, risk assessment, risk-enhancing factors, risk factors, risk reduction, risk reduction discussion, risk treatment discussion, secondhand smoke, sleep, smoking, smoking cessation, social determinants of health, socioeconomic factors, statin therapy, systems of care, tobacco, tobacco smoke pollution, treatment adherence, treatment outcomes, type 2 diabetes mellitus, waist circumference, weight loss
Preamble
Since 1980, the American College of Cardiology (ACC) and American Heart Association (AHA) have translated scientific evidence into clinical practice guidelines with recommendations to improve cardiovascular health. These guidelines, which are based on systematic methods to evaluate and classify evidence, provide a foundation for the delivery of quality cardiovascular care. The ACC and AHA sponsor the development and publication of clinical practice guidelines without commercial support, and members volunteer their time to the writing and review efforts.
Clinical practice guidelines provide recommendations applicable to patients with or at risk of developing cardiovascular disease (CVD). The focus is on medical practice in the United States, but these guidelines are relevant to patients throughout the world. Although guidelines may be used to inform regulatory or payer decisions, the goals are to improve quality of care and align with patients interests. Guidelines are intended to define practices meeting the needs of patients in most but not all circumstances and should not replace clinical judgment.
Recommendations for guideline-directed management and therapy, which encompasses clinical evaluation, diagnostic testing, and both pharmacological and procedural treatments, are effective only when adopted by both practitioners and patients. Adherence to recommendations can be enhanced by shared decision-making between clinicians and patients, with patient engagement in selecting interventions on the basis of individual values, preferences, and associated conditions and comorbidities.
The ACC/AHA Task Force on Clinical Practice Guidelines strives to ensure that the guideline writing committee includes requisite expertise and is representative of the broader medical community by selecting experts from a broad array of backgrounds, representing different geographic regions, sexes, races, ethnicities, intellectual perspectives/biases, and scopes of clinical practice. The ACC and AHA have rigorous policies and methods to ensure that documents are developed without bias or improper influence. The complete policy on relationships with industry and other entities (RWI) can be found at https://www.acc.org/guidelines/about-guidelines-and-clinical-documents/relationships-with-industry-policy.
Beginning in 2017, numerous modifications to the guidelines have been and continue to be implemented to make guidelines shorter and enhance user friendliness. Guidelines are written and presented in a modular knowledge chunk format, in which each chunk includes a table of recommendations, a brief synopsis, recommendation-specific supportive text and, when appropriate, flow diagrams or additional tables. Hyperlinked references are provided for each modular knowledge chunk to facilitate quick access and review. More structured guidelinesincluding word limits (targets) and a web guideline supplement for useful but noncritical tables and figuresare 2 such changes. This Preamble is an abbreviated version, with the detailed version available at: https://www.ahajournals.org/doi/suppl/10.1161/CIR.0000000000000677
Patrick T. OGara, MD, MACC, FAHA
Chair, ACC/AHA Task Force on Clinical Practice Guidelines
1.Introduction
Although there has been substantial improvement in atherosclerotic cardiovascular disease (ASCVD) outcomes in recent decades, ASCVD remains the leading cause of morbidity and mortality globally (S11S13). In the United States, it is also the leading cause of death for people of most racial/ethnic groups, with an estimated cost of >$200 billion annually in healthcare services, medications, and lost productivity. Much of this is attributable to suboptimal implementation of prevention strategies and uncontrolled ASCVD risk factors in many adults (S12).
Most Americans who have had a myocardial infarction (MI) had unfavorable levels of at least 1 cardiovascular risk factor before their ASCVD event (S14). In 2010, the AHA defined a new model of ideal cardiovascular health, referred to as Lifes Simple 7 (S15). Clinicians will find the 2018 Journal of American College of Cardiology (JACC) Cardiovascular Health Promotion Series very helpful in approaching the various aspects of prevention with patients (S16). An increasing number of ideal cardiovascular health factors have been associated with a lower prevalence and incidence of ASCVD events, heart failure, atrial fibrillation, cancer, depression, and cognitive impairment (S17). Therefore, moving individuals toward ideal cardiovascular health is critically important for prevention of many important health conditions.
The ACC/AHA Task Force on Clinical Practice Guidelines has commissioned this guideline to consolidate existing recommendations and various recent scientific statements, expert consensus documents, and clinical practice guidelines into a single guidance document focused on the primary prevention of ASCVD. However, this guideline also includes newly generated recommendations for aspirin use, exercise and physical activity, and tobacco use, in addition to recommendations related to team-based care, shared decision-making, and assessment of social determinants of health, to create a comprehensive yet targeted ACC/AHA guideline on the prevention of ASCVD. This guideline has been formatted in the modular chunk format to facilitate readability and future updating.
Prevention strategies occur at the population level but must also engage individual adults to slow the development of ASCVD. The most important way to prevent ASCVD is to promote a healthy lifestyle throughout life. Prevention strategies must include a strong focus on lifestyle optimization (improvements in diet, physical activity, and avoidance of tobacco use and exposure to secondhand smoke) to minimize the risk of future ASCVD events.
A comprehensive patient-centered approach that addresses all aspects of a patients lifestyle habits and estimated risk of a future ASCVD event is the first step in deciding on where there may be a need for pharmacotherapy. Even if a blood pressure (BP)reducing medication, lipid-lowering medication, or diabetes medication is ultimately prescribed, lifestyle goals should be emphasized on a regular basis. Only when a persons risk is sufficiently high should medications to reduce ASCVD risk be considered as part of a shared decision-making process for optimal treatment. In summary, clinicians and individuals should focus attention on living a healthy lifestyle by referring to these evidence-based recommendations to help prevent ASCVD.
1.1. Methodology and Evidence Review
This guideline continues the ACC and AHA effort to design a comprehensive yet succinct compilation of practical guidance for the primary prevention of ASCVD and to promote optimal dissemination of information by using concise language and formatting. The recommendations listed in this guideline are evidence based and supported by an extensive evidence review. A search for literature derived from research involving human subjects, published in English, and indexed in Ovid MEDLINE, PubMed, Cochrane Library, National Institute for Health and Care Excellence (NICE), and other selected databases relevant to this guideline, was conducted between May and July 2018. For specific search terms used and years searched per section, please see Appendix 1.
Randomized controlled trials (RCTs), systematic reviews of RCTs, meta-analyses, and large, United Statesbased, high-quality cohort studies, as well as observational studies and systematic reviews of observational studies, were evaluated for their content on the prevention of ASCVD outcomes related to the following 9 topic areas: risk assessment, diet, exercise/physical activity, obesity and weight loss, type 2 diabetes mellitus (T2DM), blood cholesterol, hypertension, smoking cessation, and aspirin use. Previous ACC/AHA guidelines, as well as U.S. Preventive Services Task Force (USPSTF) reviews and other guidance relevant to this guideline, were also assessed. The final evidence tables included in the Online Data Supplement (https://www.ahajournals.org/doi/suppl/10.1161/CIR.0000000000000677) summarize the evidence used to formulate recommendations. References selected and published in this document are representative and not all-inclusive.
Avalere Health, a healthcare advisory services firm contracted by ACC/AHA, served as the document manager for this guideline to facilitate its development process. Avalere Health commissioned the Pacific Northwest Evidence-based Practice Center at Oregon Health and Science University to perform rapid systematic evidence reviews for 5 of the key topics: aspirin use, T2DM, nutrition and diet, obesity and weight loss, and tobacco use. In parallel, an independent health data and epidemiology expert, Lee Ann Prebil, conducted a systematic evidence review for the key topic of exercise and physical activity and conducted targeted literature searches to support this documents discussion of patient-centered approaches, including team-based care, shared decision-making, and assessment of social determinants of health. A targeted literature search was also conducted for this guidelines cost and value considerations.
Recommendations and supportive text relevant to cardiovascular risk, blood cholesterol, and high BP were taken directly from 2 recently released ACC/AHA guidelines, the 2017 Hypertension Clinical Practice Guidelines (S1.11) and the 2018 Cholesterol Clinical Practice Guideline (S1.12), and were adapted for the present guideline, which aims to provide an overview of the primary prevention of ASCVD among adults. Recommendations that were adapted from previous publications are noted in the recommendation tables, and both the original published recommendation and the adapted version are provided in the guideline Web Supplement.
The results of these evidence reviews were evaluated by the writing committee for incorporation into the present guideline. (See Table S1 in the Web Supplement for a list of relevant publications and statements used in support of the guidelines recommendations.) Each topic area was assigned a primary writer, as well as a primary, and sometimes secondary, reviewer. These assignments were based on areas of particular expertise of writing committee members. All recommendations were fully reviewed and discussed among the full committee to allow for diverse perspectives and considerations for this guideline. Recommendations were then voted upon, with a modified Delphi process used to reach consensus.
1.2. Organization of the Writing Committee
The writing committee consisted of clinicians, cardiologists, health services researchers, epidemiologists, internists, nurses, and a lay representative. The writing committee included representatives from the ACC and AHA. Appendix 2 of the present document lists writing committee members relevant RWI. For the purposes of full transparency, the writing committee members comprehensive disclosure information is available online).
1.3. Document Review and Approval
This document was reviewed by 5 official reviewers nominated by the ACC and AHA (1 reviewer from the ACC/AHA Task Force for Practice Guidelines, 2 reviewers from the AHA, and 2 reviewers from the ACC); 3 reviewers on behalf of the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Society for Nutrition, and the American Society of Preventive Medicine; and 23 individual content reviewers. Reviewers RWI information was distributed to the writing committee and is published in this document (Appendix 3). This document was approved for publication by the governing bodies of the ACC and AHA.
1.4. Scope of the Guideline
This guideline is intended to be a resource for the clinical and public health practice communities. It addresses the primary prevention of CVD in adults (18 years of age), focused on outcomes of ASCVD (i.e., acute coronary syndromes, MI, stable or unstable angina, arterial revascularization, stroke, transient ischemic attack, or peripheral arterial disease of atherosclerotic origin), as well as heart failure and atrial fibrillation. The guideline presents recommendations to prevent CVD that are related to lifestyle factors (e.g., diet and exercise or physical activity), other factors affecting CVD risk (e.g., obesity, diabetes, blood cholesterol, high BP, smoking, aspirin use), patient-centered approaches (e.g., team-based care, shared decision-making, assessment of social determinants of health), and considerations of the cost and value of primary prevention.
1.5. Class of Recommendation and Level of Evidence
Recommendations are designated with both a Class of Recommendation (COR) and a Level of Evidence (LOE). The COR indicates the strength of recommendation, encompassing the estimated magnitude and certainty of benefit in proportion to risk. The LOE rates the quality of scientific evidence supporting the intervention on the basis of the type, quantity, and consistency of data from clinical trials and other sources () (S1.51).
Table 1.
Applying Class of Recommendation and Level of Evidence to Clinical Strategies, Interventions, Treatments, or Diagnostic Testing in Patient Care (Updated August 2015)
2.Overarching Recommendations for ASCVD Prevention Efforts
2.1. Patient-Centered Approaches to Comprehensive ASCVD Prevention
| Recommendations for Patient-Centered Approaches to Comprehensive ASCVD Prevention Referenced studies that support recommendations are summarized in Online Data Supplements 1and2. | ||
|---|---|---|
| COR | LOE | Recommendations |
| I | A | 1. A team-based care approach is recommended for the control of risk factors associated with ASCVD (S2.11S2.114). |
| I | B-R | 2. Shared decision-making should guide discussions about the best strategies to reduce ASCVD risk (S2.115S2.118). |
| I | B-NR | 3. Social determinants of health should inform optimal implementation of treatment recommendations for the prevention of ASCVD (S2.119S2.125). |
outlines key considerations related to social determinants of health and ASCVD prevention.
Table 2.
Example Considerations for Addressing Social Determinants of Health to Help Prevent ASCVD Events
| Topic/Domain | Example Considerations |
|---|---|
| Cardiovascular risk | Adults should be routinely assessed for psychosocial stressors and provided with appropriate counseling (S2.126). |
| Health literacy should be assessed every 4 to 6 y to maximize, recommendation effectiveness (S2.127). | |
| Diet | In addition to the prescription of diet modifications, body size perception, as well as social and cultural influences, should be assessed (S2.128, S2.129). |
| Potential barriers to adhering to a heart-healthy diet should be assessed, including food access and economic factors; these factors may be particularly relevant to persons from vulnerable populations, such as individuals residing in either inner-city or rural environments, those at socioeconomic disadvantage, and those of advanced age* (S2.130). | |
| Exercise and physical activity | In addition to the prescription of exercise, neighborhood environment and access to facilities for physical activity should be assessed (S2.131S2.133). |
| Obesity and weight loss | Lifestyle counseling for weight loss should include assessment of and interventional recommendations for psychosocial stressors, sleep hygiene, and other individualized barriers (S2.134S2.136). |
| Weight maintenance should be promoted in patients withoverweight/obesity who are unable to achieve recommended weight loss. | |
| Diabetes mellitus | In addition to the prescription of type 2 diabetes mellitusinterventions, environmental and psychosocial factors, including depression, stress, self-efficacy, and social support, should be assessed to improve achievement of glycemic control and adherence to treatment (S2.137S2.140). |
| High blood pressure | Short sleep duration (<6 h) and poor-quality sleep are associated with high blood pressure and should be considered (S2.141). Because other lifestyle habits can impact blood pressure, access to a healthy, low-sodium diet and viable exercise options should also be considered. |
| Tobacco treatment | Social support is another potential determinant of tobacco use.Therefore, in adults who use tobacco, assistance and arrangement for individualized and group social support counseling are recommended (S2.142, S2.143). |
2.2. Assessment of Cardiovascular Risk
| Recommendations for Assessment of Cardiovascular Risk Referenced studies that support recommendations are summarized in Online Data Supplement 3. | ||
|---|---|---|
| COR | LOE | Recommendations |
| I | B-NR | 1. For adults 40 to 75 years of age, clinicians should routinely assess traditional cardiovascular risk factors and calculate 10-year risk of ASCVD by using the pooled cohort equations (PCE) (S2.21, S2.22). |
| IIa | B-NR | 2. For adults 20 to 39 years of age, it is reasonable to assess traditional ASCVD risk factors at least every 4 to 6 years (S2.21S2.23). |
| IIa | B-NR | 3. In adults at borderline risk (5% to <7.5% 10-year ASCVD risk) or intermediate risk (7.5% to <20% 10-year ASCVD risk), it is reasonable to use additional riskenhancing factors to guide decisions about preventive interventions (e.g., statin therapy) (S2.24S2.214). |
| IIa | B-NR | 4. In adults at intermediate risk (7.5% to <20% 10-year ASCVD risk) or selected adults at borderline risk (5% to <7.5% 10-year ASCVD risk), if risk-based decisions for preventive interventions (e.g., statin therapy) remain uncertain, it is reasonable to measure a coronary artery calcium score to guide clinicianpatient risk discussion (S2.215S2.231). |
| IIb | B-NR | 5. For adults 20 to 39 years of age and for those 40 to 59 years of age who have <7.5% 10-year ASCVD risk, estimating lifetime or 30-year ASCVD risk may be considered (S2.21, S2.22, S2.232S2.235). |
Among adults at borderline (5% to <7.5%) and intermediate (7.5% to <20%) risk, one may consider additional individual risk-enhancing clinical factors () that can be used to revise the 10-year ASCVD risk estimate (S2.24). These factors may include having a family history of premature ASCVD (S2.25), chronic inflammatory disease [rheumatoid arthritis (S2.26), lupus (S2.27), or HIV infection (S2.212)], South Asian ancestry (S2.213), a history of preeclampsia (S2.28) or preterm delivery (S2.29), early menopause (S2.210), erectile dysfunction (S2.211), chronic kidney disease (CKD), metabolic syndrome, persistently elevated inflammatory markers (S2.214), or elevated lipid biomarkers (S2.24). After these clinically available risk-enhancing factors have been considered, if there is still uncertainty about the reliability of the risk estimate for individuals in the borderline- or intermediate-risk categories, further testing to document subclinical coronary atherosclerosis is reasonable to more accurately reclassify the risk estimate upward or downward (S2.217S2.219, S2.236).
Table 3.
Risk-Enhancing Factors for ClinicianPatient Risk Discussion
| Risk-Enhancing Factors |
|---|
| Family history of premature ASCVD (males, age <55 y; females, age <65 y) |
| Primary hypercholesterolemia (LDL-C 160189 mg/dL [4.14.8 mmol/L]; nonHDL-C 190219 mg/dL [4.95.6 mmol/L])* |
| Metabolic syndrome (increased waist circumference [by ethnically appropriate cutpoints], elevated triglycerides [>150 mg/dL, nonfasting], elevated blood pressure, elevated glucose, and low HDL-C [<40 mg/dL in men; <50 mg/dL in women] are factors; a tally of 3 makes the diagnosis) |
| Chronic kidney disease (eGFR 1559 mL/min/1.73 m2 with or without albuminuria; not treated with dialysis or kidney transplantation) |
| Chronic inflammatory conditions, such as psoriasis, RA, lupus, or HIV/AIDS |
| History of premature menopause (before age 40 y) and history of pregnancy-associated conditions that increase later ASCVD risk, such as preeclampsia |
| High-risk race/ethnicity (e.g., South Asian ancestry) |
| Lipids/biomarkers: associated with increased ASCVD risk Persistently elevated* primary hypertriglyceridemia (175 mg/dL, nonfasting); |
| If measured: |
| Elevated high-sensitivity C-reactive protein (2.0 mg/L) |
| Elevated Lp(a): A relative indication for its measurement is family history of premature ASCVD. An Lp(a) 50 mg/dL or 125 nmol/L constitutes a risk-enhancing factor, especially at higher levels of Lp(a). |
| Elevated apoB (130 mg/dL): A relative indication for its measurement would be triglyceride 200 mg/dL. A level >130 mg/dL corresponds to an LDL-C 160 mg/dL and constitutes a risk-enhancing factor |
| ABI (<0.9) |
3.Lifestyle Factors Affecting Cardiovascular Risk
3.1. Nutrition and Diet
| Recommendations for Nutrition and Diet Referenced studies that support recommendations are summarized in Online Data Supplements 4and5. | ||
|---|---|---|
| COR | LOE | Recommendations |
| I | B-R | 1. A diet emphasizing intake of vegetables, fruits, legumes, nuts, whole grains, and fish is recommended to decrease ASCVD risk factors (S3.11S3.111). |
| IIa | B-NR | 2. Replacement of saturated fat with dietary monounsaturated and polyunsaturated fats can be beneficial to reduce ASCVD risk (S3.112, S3.113). |
| IIa | B-NR | 3. A diet containing reduced amounts of cholesterol and sodium can be beneficial to decrease ASCVD risk (S3.19, S3.114S3.116). |
| IIa | B-NR | 4. As a part of a healthy diet, it is reasonable to minimize the intake of processed meats, refined carbohydrates, and sweetened beverages to reduce ASCVD risk (S3.117S3.123). |
| III-Harm | B-NR | 5. As a part of a healthy diet, the intake of trans fats should be avoided to reduce ASCVD risk (S3.112, S3.117, S3.125S3.127). |
3.2. Exercise and Physical Activity
| Recommendations for Exercise and Physical Activity Referenced studies that support recommendations are summarized in Online Data Supplements 6and7. | ||
|---|---|---|
| COR | LOE | Recommendations |
| I | B-R | 1. Adults should be routinely counseled in healthcare visits to optimize a physically active lifestyle (S3.21, S3.22). |
| I | B-NR | 2. Adults should engage in at least 150 minutes per week of accumulated moderate-intensity or 75 minutes per week of vigorous-intensity aerobic physical activity (or an equivalent combination of moderate and vigorous activity) to reduce ASCVD risk (S3.23S3.28). |
| IIa | B-NR | 3. For adults unable to meet the minimum physical activity recommendations (at least 150 minutes per week of accumulated moderate-intensity or 75 minutes per week of vigorous-intensity aerobic physical activity), engaging in some moderate- or vigorous-intensity physical activity, even if less than this recommended amount, can be beneficial to reduce ASCVD risk (S3.25, S3.26). |
| IIb | C-LD | 4. Decreasing sedentary behavior in adults may be reasonable to reduce ASCVD risk (S3.23, S3.29S3.211). |
Other activity states that comprise a 24-hour period for an average individual include sleep, light-intensity physical activity, and sedentary behavior (). Sedentary behavior refers to waking behavior with an energy expenditure of 1.5 metabolic equivalents while in a sitting or reclining posture () (S3.212).
Hours Per Day Spent in Various States of ActivityU.S. adults spend >7 h/d on average in sedentary activities. Replacing sedentary time with other physical activity involves increasing either moderate- to vigorous-intensity physical activity or light-intensity physical activity.
Data modified from Young et al. (S3.212).
Table 4.
Definitions and Examples of Different Intensities of Physical Activity
| Intensity | METs | Examples |
|---|---|---|
| Sedentary behavior* | 11.5 | Sitting, reclining, or lying; watching television |
| Light | 1.62.9 | Walking slowly, cooking, light housework |
| Moderate | 3.05.9 | Brisk walking (2.44 mph), biking (59 mph), ballroom dancing, active yoga, recreational swimming |
| Vigorous | 6 | Jogging/running, biking (10 mph), singles tennis, swimming laps |
4.Other Factors Affecting Cardiovascular Risk
4.1. Adults With Overweight and Obesity
| Recommendations for Adults With Overweight and Obesity Referenced studies that support recommendations are summarized in Online Data Supplements 8and9. | ||
|---|---|---|
| COR | LOE | Recommendations |
| I | B-R | 1. In individuals with overweight and obesity, weight loss is recommended to improve the ASCVD risk factor profile (S4.11). |
| I | B-R | 2. Counseling and comprehensive lifestyle interventions, including calorie restriction, are recommended for achieving and maintaining weight loss in adults with overweight and obesity (S4.11, S4.12). |
| I | C-EO | 3. Calculating body mass index (BMI) is recommended annually or more frequently to identify adults with overweight and obesity for weight loss considerations. |
| IIa | B-NR | 4. It is reasonable to measure waist circumference to identify those at higher cardiometabolic risk (S4.13S4.16). |
4.2. Adults With Type 2 Diabetes Mellitus
See for an algorithm for treatment of T2DM for primary prevention of cardiovascular disease.
Treatment of T2DM for Primary Prevention of Cardiovascular DiseaseCVD indicates cardiovascular disease; GLP-1R, glucagon-like peptide-1 receptor; HbA1c, hemoglobin A1c; SGLT-2, sodium-glucose cotransporter 2; and T2DM, type 2 diabetes mellitus.
| Recommendations for Adults With Type 2 Diabetes Mellitus Referenced studies that support recommendations are summarized in Online Data Supplement 10. | ||
|---|---|---|
| COR | LOE | Recommendations |
| I | A | 1. For all adults with T2DM, a tailored nutrition plan focusing on a heart-healthy dietary pattern is recommended to improve glycemic control, achieve weight loss if needed, and improve other ASCVD risk factors (S4.21, S4.22). |
| I | A | 2. Adults with T2DM should perform at least 150 minutes per week of moderate-intensity physical activity or 75 minutes of vigorous-intensity physical activity to improve glycemic control, achieve weight loss if needed, and improve other ASCVD risk factors (S4.23, S4.24). |
| IIa | B-R | 3. For adults with T2DM, it is reasonable to initiate metformin as first-line therapy along with lifestyle therapies at the time of diagnosis to improve glycemic control and reduce ASCVD risk (S4.25S4.28). |
| IIb | B-R | 4. For adults with T2DM and additional ASCVD risk factors who require glucose-lowering therapy despite initial lifestyle modifications and metformin, it may be reasonable to initiate a sodium-glucose cotransporter 2 (SGLT-2) inhibitor or a glucagon-like peptide-1 receptor (GLP-1R) agonist to improve glycemic control and reduce CVD risk (S4.29S4.214). |
4.3. Adults With High Blood Cholesterol
Recommendations from the 2018 Cholesterol Clinical Practice Guidelines (S4.31) are included and adapted below.
| Recommendations for Adults With High Blood Cholesterol Referenced studies that support recommendations are summarized in Online Data Supplements 11and12. | ||
|---|---|---|
| COR | LOE | Recommendations |
| I | A | 1. In adults at intermediate risk (7.5% to <20% 10-year ASCVD risk), statin therapy reduces risk of ASCVD, and in the context of a risk discussion, if a decision is made for statin therapy, a moderate-intensity statin should be recommended (S4.32S4.39).Adapted from recommendations in the 2018 Cholesterol Clinical Practice Guidelines (S4.31). |
| I | A | 2. In intermediate risk (7.5% to <20% 10-year ASCVD risk) patients, LDL-C levels should be reduced by 30% or more, and for optimal ASCVD risk reduction, especially in patients at high risk (20% 10-year ASCVD risk), levels should be reduced by 50% or more (S4.32, S4.35S4.310).Adapted from recommendations in the 2018 Cholesterol Clinical Practice Guidelines (S4.31). |
| I | A | 3. In adults 40 to 75 years of age with diabetes, regardless of estimated 10-year ASCVD risk, moderate-intensity statin therapy is indicated (S4.311S4.319). Included from recommendations in the 2018 Cholesterol Clinical Practice Guidelines (S4.31). |
| I | B-R | 4. In patients 20 to 75 years of age with an LDL-C level of 190 mg/dL (4.9 mmol/L) or higher, maximally tolerated statin therapy is recommended (S4.32, S4.320S4.325).Included from recommendations in the 2018 Cholesterol Clinical Practice Guidelines (S4.31). |
| IIa | B-R | 5. In adults with diabetes mellitus who have multiple ASCVD risk factors, it is reasonable to prescribe high-intensity statin therapy with the aim to reduce LDL-C levels by 50% or more (S4.32, S4.37). Included from recommendations in the 2018 Cholesterol Clinical Practice Guidelines (S4.31). |
| IIa | B-R | 6. In intermediate-risk (7.5% to <20% 10-year ASCVD risk) adults, risk-enhancing factors favor initiation or intensification of statin therapy (S4.37, S4.326S4.333).Adapted from recommendations in the 2018 Cholesterol Clinical Practice Guidelines (S4.31). |
| IIa | B-NR | 7. In intermediate-risk (7.5% to <20% 10-year ASCVD risk) adults or selected borderline-risk (5% to <7.5% 10-year ASCVD risk) adults in whom a coronary artery calcium score is measured for the purpose of making a treatment decision, AND If the coronary artery calcium score is zero, it is reasonable to withhold statin therapy and reassess in 5 to 10 years, as long as higher-risk conditions are absent (e.g., diabetes, family history of premature CHD, cigarette smoking); If coronary artery calcium score is 1 to 99, it is reasonable to initiate statin therapy for patients 55 years of age; If coronary artery calcium score is 100 or higher or in the 75th percentile or higher, it is reasonable to initiate statin therapy (S4.328, S4.334). Adapted from recommendations in the 2018 Cholesterol Clinical Practice Guidelines (S4.31). |
| IIb | B-R | 8. In patients at borderline risk (5% to <7.5% 10-year ASCVD risk), in risk discussion, the presence of risk-enhancing factors may justify initiation of moderate-intensity statin therapy (S4.328, S4.335). Adapted from recommendations in the 2018 Cholesterol Clinical Practice Guidelines (S4.31). |
Primary ASCVD prevention requires attention to ASCVD risk factors beginning early in life (). The benefit from statin therapy is related to both global risk and intensity of treatment (S4.32), and no RCTs of high-intensity statin therapy have been carried out in cohorts of patients exclusively with diabetes. On the basis of these considerations and the fact that patients with diabetes have a higher trajectory of lifetime risk than do those without diabetes, high-intensity statin therapy is preferred in patients with diabetes as they develop risk modifiers ().
Primary PreventionColors correspond to Class of Recommendation in Table 1.
ABI indicates ankle-brachial index; apoB, apolipoprotein B; ASCVD, atherosclerotic cardiovascular disease; CAC, coronary artery calcium; CHD, coronary heart disease; HIV, human immunodeficiency virus; hs-CRP, high-sensitivity C-reactive protein; LDL-C, low-density lipoprotein cholesterol; and Lp(a), lipoprotein (a). </p/> Reproduced with permission from Grundy et al. (S4.31). Copyright 2018, American Heart Association, Inc., and American College of Cardiology Foundation.
Table 5.
Diabetes-Specific Risk Enhancers That Are Independent of Other Risk Factors in Diabetes Mellitus
| Risk Enhancers in Diabetic Patients |
|---|
| Long duration (10 years for T2DM (S4.336) or 20 years for type 1 diabetes mellitus (S4.316)) |
| Albuminuria 30 mcg albumin/mg creatinine (S4.337) |
| eGFR <60 mL/min/1.73 m2(S4.337) |
| Retinopathy (S4.338) |
| Neuropathy (S4.339) |
| ABI <0.9 (S4.340, S4.341) |
Selected examples of candidates who might benefit from knowing their coronary artery calcium score is zero are listed in .
Table 6.
Selected Examples of Candidates for Coronary Artery Calcium Measurement Who Might Benefit From Knowing Their Coronary Artery Calcium Score Is Zero
| Coronary Artery Calcium Measurement Candidates Who Might Benefit from Knowing Their Coronary Artery Calcium Score Is Zero |
|---|
| Patients reluctant to initiate statin who wish to understand their risk and potential for benefit more precisely |
| Patients concerned about need to reinstitute statin therapy after discontinuation for statin-associated symptoms |
| Older patients (men 5580 y of age; women 6080 y of age) with low burden of risk factors (S4.442) who question whether they would benefit from statin therapy |
| Middle-aged adults (4055 y of age) with PCE-calculated 10-year risk for ASCVD 5% to <7.5% with factors that increase their ASCVD risk, although they are in a borderline risk group. |
4.4. Adults With High Blood Pressure or Hypertension
Recommendations from the 2017 Hypertension Clinical Practice Guidelines (S4.41) are adapted below.
| Recommendations for Adults With High Blood Pressure or Hypertension Referenced studies that support recommendations are summarized in Online Data Supplements 13and14. | ||
|---|---|---|
| COR | LOE | Recommendations |
| I | A | 1. In adults with elevated blood pressure (BP) or hypertension, including those requiring antihypertensive medications nonpharmacological interventions are recommended to reduce BP. These include: weight loss (S4.42S4.45); a heart-healthy dietary pattern (S4.46S4.48); sodium reduction (S4.49S4.413); dietary potassium supplementation (S4.414S4.418); increased physical activity with a structured exercise program (S4.43, S4.45, S4.411, S4.419S4.423); and limited alcohol (S4.424S4.429).Adapted from recommendations in the 2017 Hypertension Clinical Practice Guidelines (S4.41). |
| I | SBP: A | 2. In adults with an estimated 10-year ASCVD risk* of 10% or higher and an average systolic BP (SBP) of 130 mm Hg or higher or an average diastolic BP (DBP) of 80 mm Hg or higher, use of BP-lowering medications is recommended for primary prevention of CVD (S4.430S4.438).Adapted from recommendations in the 2017 Hypertension Clinical Practice Guidelines (S4.41). |
| DBP: C-EO | ||
| I | SBP: B-RSR | 3. In adults with confirmed hypertension and a 10-year ASCVD event risk of 10% or higher, a BP target of less than 130/80 mm Hg is recommended (S4.433, S4.439S4.442).Adapted from recommendations in the 2017 Hypertension Clinical Practice Guidelines (S4.41). |
| DBP: C-EO | ||
| I | SBP: B-RSR | 4. In adults with hypertension and chronic kidney disease, treatment to a BP goal of less than 130/80 mm Hg is recommended (S4.443S4.448).Adapted from recommendations in the 2017 Hypertension Clinical Practice Guidelines (S4.41). |
| DBP: C-EO | ||
| I | SBP: B-RSR | 5. In adults with T2DM and hypertension, antihypertensive drug treatment should be initiated at a BP of 130/80 mm Hg or higher, with a treatment goal of less than 130/80 mm Hg (S4.433, S4.447, S4.449S4.454).Adapted from recommendations in the 2017 Hypertension Clinical Practice Guidelines (S4.41). |
| DBP: C-EO | ||
| I | C-LD | 6. In adults with an estimated 10-year ASCVD risk <10% and an SBP of 140 mm Hg or higher or a DBP of 90 mm Hg or higher, initiation and use of BP-lowering medication are recommended (S4.436, S4.455S4.458).Adapted from recommendations in the 2017 Hypertension Clinical Practice Guidelines (S4.41). |
| IIb | SBP: B-NR | 7. In adults with confirmed hypertension without additional markers of increased ASCVD risk, a BP target of less than 130/80 mm Hg may be reasonable (S4.459S4.462).Adapted from recommendations in the 2017 Hypertension Clinical Practice Guidelines (S4.41). |
| DBP: C-EO |
See for the BP thresholds and treatment recommendations algorithm and refer to the 2017 Hypertension Clinical Practice Guidelines for comprehensive details (S4.41).
BP Thresholds and Recommendations for TreatmentColors correspond to Class of Recommendation in .
BP indicates blood pressure; and CVD, cardiovascular disease. </p/> Adapted with permission from Whelton et al. (S4.41). Copyright 2017, American College of Cardiology Foundation and the American Heart Association, Inc.
See for recommended dose and approximate impact on SBP.
Table 7.
Best Proven Nonpharmacological Interventions for Prevention and Treatment of Hypertension*
| NonpharmacologicalIntervention | Goal | Approximate Impact on SBP | |||
|---|---|---|---|---|---|
| Hypertension | Normotension | Reference | |||
| Weight loss | Weight/body fat | Best goal is ideal body weight, but aim for at least a 1-kg reduction in body weight for most adults who are overweight. Expect about1 mm Hg for every 1-kg reduction in body weight. | 5 mm Hg | 2/3 mm Hg | (S4.42) |
| Healthy diet | DASH dietary pattern | Consume a diet rich in fruits, vegetables, whole grains, and low-fat dairy products, with reduced content of saturated and total fat. | 11 mm Hg | 3 mm Hg | (S4.47, S4.48) |
| Reduced intake of dietary sodium | Dietary sodium | Optimal goal is <1500 mg/d, but aim for at least a 1000-mg/d reduction in most adults. | 5/6 mm Hg | 2/3 mm Hg | (S4.412, S4.410) |
| Enhanced intake of dietary potassium | Dietary potassium | Aim for 35005000 mg/d, preferably by consumption of a diet rich in potassium. | 4/5 mm Hg | 2 mm Hg | (S4.414) |
| Physical activity | Aerobic | 90150 min/wk 65%75% heart rate reserve | 5/8 mm Hg | 2/4 mm Hg | (S4.419, S4.420) |
| Dynamic resistance | 90150 min/wk 50%80% 1 rep maximum 6 exercises, 3 sets/exercise, 10 repetitions/set | 4 mm Hg | 2 mm Hg | (S4.419) | |
| Isometric resistance | 4 2 min (hand grip), 1 min rest between exercises, 30%40% maximum voluntary contraction, 3 sessions/wk 810 wk | 5 mm Hg | 4 mm Hg | (S4.421, S4.463) | |
| Moderation in alcohol intake | Alcohol consumption | In individuals who drink alcohol, reduce alcohol to: Men: 2 drinks daily Women: 1 drink daily | 4 mm Hg | 3 mm Hg | (S4.420, 54.4 24, 54.425) |
4.5. Treatment of Tobacco Use
| Recommendations for Treatment of Tobacco Use Referenced studies that support recommendations are summarized in Online Data Supplements 15and16. | ||
|---|---|---|
| COR | LOE | Recommendations |
| I | A | 1. All adults should be assessed at every healthcare visit for tobacco use and their tobacco use status recorded as a vital sign to facilitate tobacco cessation (S4.51). |
| I | A | 2. To achieve tobacco abstinence, all adults who use tobacco should be firmly advised to quit (S4.52). |
| I | A | 3. In adults who use tobacco, a combination of behavioral interventions plus pharmacotherapy is recommended to maximize quit rates (S4.52,S4.53). |
| I | B-NR | 4. In adults who use tobacco, tobacco abstinence is recommended to reduce ASCVD risk (S4.54, S4.55). |
| IIa | B-R | 5. To facilitate tobacco cessation, it is reasonable to dedicate trained staff to tobacco treatment in every healthcare system (S4.51). |
| III: Harm | B-NR | 6. All adults and adolescents should avoid secondhand smoke exposure to reduce ASCVD risk (S4.56). |
In alignment with previous expert consensus regarding strategies for tobacco cessation (S4.57), summarizes recommended behavioral interventions and pharmacotherapy for tobacco treatment. There are 7 FDA-approved cessation medications, including 5 forms of nicotine replacement. Note that the black box warnings about neuropsychiatric events have been removed by the FDA (S4.58, 4.59).
Table 8.
Highlights of Recommended Behavioral and Pharmacotherapy Tobacco Treatment Modalities for Prescribers*
| Timing of Behavioral Interventions | |||
| <3 min of tobacco status assessment with cessation counseling at each clinic encounter | >310 min of tobacco status assessment with cessation counseling at each clinic encounter | >10 min of tobacco status assessment with cessation counseling at each clinic encounter | |
| Treatment | Dosing | Precautions | |
| NRT* | |||
| Patch | 21 mg, 14 mg, or 7 mg | Starting dose:21 mg for >10 CPD; 14 mg for <10 CPD | Local irritation possible; avoid with skin disorders; may remove for sleep if needed |
| Gum | 2 mg or 4 mg | Starting dose:4 mg if first tobacco use is <30 min after waking; 2 mg if first tobacco use is >30 min after waking; maximum of 20 lozenges or 24 pieces of gum/d.Chew and park gum* | Hiccups/dyspepsia possible; avoid food or beverages 15 min before and after use |
| Lozenge | 2 mg or 4 mg | ||
| Nasal spray | 10 mg/mL | Starting dose:12 doses/h (1 dose=2 sprays); maximum of 40 doses/d | Local irritation possible; avoid with nasal or reactive airway disordersAmerican |
| Oral inhaler | 10, 10-mg cartridge | Starting dose:Puff for 20 min/cartridge every 12 h; maximum 616 cartridges/d; taper over 36 mo | Cough possible; avoid with reactive airway disorders |
| Other|| | |||
| Bupropion (Zyban [GlaxoSmithKline], | 150 mg | 150 mg once daily (am) for 3 d; then 150 mg twice daily; may use | Avoid with history/risk of seizures, eating disorders, MAO inhibitors, or |
| Wellbutrin SR [GlaxoSmithKline]) | SR | in combination with NRT (S4.59) | CYP 2D6 inhibitor |
| Varenicline (Chantix [Pfizer]) | 0.5 mg or 1 mg | 0.5 mg once daily (am) for 3 d; then 0.5 mg twice daily for 4 d; then 1 mg twice daily (use start pack followed by continuation pack) for 36 mo | Nausea common; take with food. Renal dosing required. Very limited drug interactions; near-exclusive renal clearance. |
4.6. Aspirin Use
| Recommendations for Aspirin Use Referenced studies that support recommendations are summarized in Online Data Supplements 17and18. | ||
|---|---|---|
| COR | LOE | Recommendations |
| IIb | A | 1. Low-dose aspirin (75100 mg orally daily) might be considered for the primary prevention of ASCVD among select adults 40 to 70 years of age who are at higher ASCVD risk but not at increased bleeding risk (S4.61S4.68). |
| III: Harm | B-R | 2. Low-dose aspirin (75100 mg orally daily) should not be administered on a routine basis for the primary prevention of ASCVD among adults >70 years of age (S4.69). |
| III: Harm | C-LD | 3. Low-dose aspirin (75100 mg orally daily) should not be administered for the primary prevention of ASCVD among adults of any age who are at increased risk of bleeding (S4.610). |
5.Cost and Value Considerations
The growing need to consider value stems directly from the goal of achieving the best possible health outcomes with finite healthcare resources in the primary prevention of CVD (S51). Value in healthcare can be defined as the incremental health benefits of a therapy or procedure relative to its incremental net long-term costs. The consideration of cost and value in the guideline development process supports key goals, including: 1) enhancing overall value in the delivery of cardiovascular care and 2) involving healthcare professionals in the challenging care decisions that must be made to increase value in the U.S. healthcare system (S52).
The integration of value assessments into our national guidelines involves inherent methodological challenges, including: 1) variability in costs across different healthcare settings, 2) variability in costs and benefits across different patient subgroups, 3) variability over time, 4) variability in who bears the burden of the health outcome (i.e., typically the individual patient) versus who bears the burden of the healthcare cost (e.g., often spread beyond the individual to third-party payers, taxpayers), and 5) an inadequate literature base on which to render a sound, evidence-based assessment of certain specific therapies (S51, S52).
There are additional challenges specific to the prevention realm. As described in the 2011 AHA policy statement, Value of Primordial and Primary Prevention in CVD (S51):
Assessing the value of prevention in apparently healthy patients is generally more difficult than evaluating therapy for established disease because the time horizon to the clinical manifestation of disease is generally longmany decades in the young. Thus, it is difficult, perhaps impossible, to assess long-term effectiveness in terms of survival or quality-adjusted life-years (QALYs) or associated costs because of increasing uncertainty about outcome the further one tries to look into the future.
Furthermore, the principle of discounting, which places relative emphasis on current costs and benefits while deemphasizing downstream costs and benefits, creates disadvantages for prevention because costs often accrue in the present while the benefit may only be fully realized long into the future. These methodological challenges notwithstanding, prior AHA statements have highlighted the public policies, community efforts, and pharmacological interventions that are likely to be cost-effective and, at times, cost-saving prevention tactics compared with common benchmarks. For example, robust evidence suggests that both antihypertensive therapy (S53S56) and statin therapy (S57S59), particularly with low-cost generic drug formulations, are high-value interventions across a wide spectrum of risk and age strata.
The incorporation of the value category into clinical practice guidelines is one of several considerations in medical decision-making and resource allocation. Clinicians, researchers, and policymakers alike must continue to place cost-effective analyses in the proper context, extracting key value determinations while acknowledging the challenges in fully characterizing and incorporating the downstream benefits of a given therapeutic prevention tactic. Further research and methodological advances are needed to comprehensively characterize the full spectrum of benefits produced by the prevention approach, thereby rendering cost-effectiveness assessments more consequential to clinical practice.
6.Conclusion
Most ASCVD events are avoidable through primordial prevention (i.e., the prevention of risk factor development) and control of traditional cardiovascular risk factors. Tobacco avoidance is critically important for ASCVD prevention, and all adults should strive to engage in regular brisk physical activity most days of the week and adhere to a healthy dietary pattern to help lower future ASCVD risk. A diet high in fruits, vegetables, and whole grains is best. Fish, legumes, and poultry are the preferred sources of protein. Minimizing the consumption of trans fats, added sugars (including sugar-sweetened beverages), red meats, sodium, and saturated fats is also important. Clinicians should work in partnership with patients to assess their readiness for sustained lifestyle improvements, identify potential barriers to change, and encourage them to try to achieve measurable goals and continue to monitor their progress (S61). Finally, social determinants of ASCVD riskand their impact on the patients ability to prevent or treat risk factorsmust be taken into account. Clinicians need to consider patients health literacy and education levels and assess patients motivation to improve their lifestyle habits.
The goal of the clinician is to match the intensity of preventive efforts with an individuals absolute risk of a future ASCVD event and with the individuals willingness and capacity to implement preventive strategies. Risk estimation is imperfect and based on group averages that are then applied to individual patients. The clinician must balance an understanding of a patients estimated ASCVD risk with potential benefits and adverse risk from pharmacological therapy in the context of a risk discussion. To determine the appropriateness of pharmacological therapy after quantitative risk estimation in cases that are unclear, risk-enhancing factors or selective use of a coronary artery calcium measurement can inform decision-making for cholesterol-lowering or antihypertensive medication use in intermediate-risk individuals.
This primary-prevention guideline strives to provide clinicians with the information they need to help their patients reduce their risk of ASCVD and encourage them to make healthier lifestyle changes when needed.
Supplementary Material
targeted literature searches
comprehensive relationships table
ACC/AHA TASK FORCE MEMBERS
Patrick T. OGara, MD, MACC, FAHA, Chair, Joshua A. Beckman, MD, MS, FAHA, Chair-Elect, Glenn N. Levine, MD, FACC, FAHA, Immediate Past Chair, Sana M. Al-Khatib, MD, MHS, FACC, FAHA Mark A. Hlatky, MD, FACC, FAHA, Kim K. Birtcher, PharmD, MS, AACC John Ikonomidis, MD, PhD, FAHA, Joaquin E. Cigarroa, MD, FACC Jos A. Joglar, MD, FACC, FAHA, Anita Deswal, MD, MPH, FACC, FAHA Laura Mauri, MD, MSc, FAHA, Lee A. Fleisher, MD, FACC, FAHA Mariann R. Piano, RN, PhD, FAHA, Federico Gentile, MD, FACC Barbara Riegel, PhD, RN, FAHA, Zachary D. Goldberger, MD, MS, FACC, FAHA Duminda N. Wijeysundera, MD, PhD
1.6.Abbreviations
Abbreviation Meaning/Phrase
| ASCVD | atherosclerotic cardiovascular disease |
| AU | Agatston units |
| BMI | body mass index |
| BP | blood pressure |
| CHD | coronary heart disease |
| CKD | chronic kidney disease |
| CVD | cardiovascular disease |
| DASH | Dietary Approaches to Stop Hypertension |
| DBP | diastolic blood pressure |
| DM | diabetes mellitus |
| ENDS | electronic nicotine delivery systems |
| FDA | U.S. Food and Drug Administration |
| GLP-1R | glucagon-like peptide-1 receptor |
| HbA1c | hemoglobin A1c |
| HDL-C | High-density lipoprotein cholesterol |
| HbA1c | hemoglobin A1c |
| LDL-C | low-density lipoprotein cholesterol |
| MI | myocardial infarction |
| PCE | pooled cohort equations |
| RCT | randomized controlled trial |
| SBP | systolic blood pressure |
| SGLT-2 | sodium-glucose cotransporter 2 |
| T2DM | type 2 diabetes mellitus |
| USPSTF | U.S. Preventive Services Task Force |
Appendix 1.Search Criteria
The rapid review conducted by the Evidence-based Practice Center to complete this literature search, in the limited timeframe provided, built on existing systematic reviews conducted on behalf of the USPSTF.
| Medical Subject Headings (MeSH) Terms | Key Words |
|---|---|
| Nutrition and Diet | |
| Search since the 2017 review (1) | |
| exp Diet/ | diet* |
| exp Diet Therapy/ | cardiovascular |
| Healthy Diet | coronary |
| Primary Prevention/ | heart |
| myocardial infarction | |
| MI | |
| CVD | |
| CHD | |
| cerebrovascular | |
| stroke | |
| microvascular | |
| mortality | |
| prevent* | |
| Obesity and Weight Loss | |
| Search since the 2018 review (2) | |
| exp Obesity/ | obes* |
| exp Weight Loss | overweight |
| Primary Prevention/ | weight |
| cardiovascular | |
| coronary | |
| heart | |
| myocardial infarction | |
| MI | |
| CVD | |
| CHD | |
| cerebrovascular | |
| stroke | |
| microvascular | |
| mortality | |
| prevent* | |
| Type 2 Diabetes Mellitus | |
| Search since the 2015 review (3) | |
| exp Diabetes Mellitus, Type 2/ | impaired fasting glucose |
| Prediabetic State/ | impaired glucose tolerance |
| Glucose Intolerance/ | Ifg |
| Primary Prevention/ | Igt |
| prediabetes* | |
| type 2 diabet* | |
| DM | |
| cardiovascular | |
| coronary | |
| heart | |
| myocardial infarction | |
| MI | |
| CVD | |
| CHD | |
| cerebrovascular | |
| stroke | |
| microvascular | |
| mortality | |
| prevent* | |
| Tobacco Use | |
| Search since the 2015 review (4) | |
| Smoking/ | smoking |
| exp Tobacco Use Cessation/ | cigarette* |
| Tobacco Use Disorder/ | tobacco |
| Electronic Cigarettes/ | nicotine |
| Primary Prevention/ | vape |
| vaping | |
| e-cigarette | |
| electronic cigarette | |
| electronic nicotine delivery system* | |
| ENDS | |
| cardiovascular | |
| coronary | |
| heart | |
| myocardial infarction | |
| MI | |
| CVD | |
| CHD | |
| cerebrovascular | |
| stroke | |
| microvascular | |
| mortality | |
| prevent* | |
| Aspirin Use | |
| Search since the 2016 review (5) | |
| Aspirin | aspirin |
| exp Cerebrovascular Disorders/ | acetylsalicylic acid |
| exp Cardiovascular Diseases/ | clopidogrel |
| Primary Prevention/ | cardiovascular |
| coronary | |
| heart | |
| myocardial infarction | |
| MI | |
| CVD | |
| CHD | |
| cerebrovascular | |
| stroke | |
| microvascular | |
| mortality | |
| prevent* | |
| Social Determinants of Health | |
| Search limited to English. No date restrictions (conducted 7/11/2018) Similar articles searches were also conducted where potentially highly relevant papers were found | |
| NONE SPECIFIED, BUT DUE TO AUTOMATIC TERM MAPPING IN PUBMED, SOME MeSH TERMS MAY HAVE BEEN EMPLOYED | Social determinants of health |
| Equity | |
| Social status | |
| Social deprivation | |
| Neighborhood | |
| Neighborhood conditions | |
| Uninsured | |
| Housing | |
| Immigration | |
| Adverse childhood events | |
| Social gradient | |
| Educational status | |
| Inequalities | |
| Sexuality | |
| Atherosclerosis | |
| cardiovascular | |
| Team Based Care | |
| Search limited to English, 1/1/201010/14/2018 (though earlier articles may have been identified through related articles search)Related articles searches were also conducted where potentially highly relevant papers were found | |
| NONE SPECIFIED, BUT DUE TO AUTOMATIC TERM MAPPING IN PUBMED, SOME MeSH TERMS MAY HAVE BEEN EMPLOYED | team |
| Team care | |
| Collaborative care | |
| Multidisciplinary | |
| team based | |
| team approach | |
| prevention | |
| Primary prevention | |
| Cardiovascular disease, | |
| Cholesterol | |
| Aspirin | |
| Smoking | |
| Obesity | |
| Heart disease | |
| Atherosclerosis | |
| stroke | |
| Shared Decision Making | |
| Search limited to English, 1/1/201010/24/2018 (though earlier articles may have been identified through related articles search)Related articles searches were also conducted where potentially highly relevant papers were found | |
| NONE SPECIFIED, BUT DUE TO AUTOMATIC TERM MAPPING IN PUBMED, SOME MeSH TERMS MAY HAVE BEEN AUTOMATICALLY EMPLOYED | Shared decision making |
| Prevention | |
| Cardiovascular | |
| Atherosclerosis | |
| Stroke | |
| Heart | |
| Hypertension | |
| Lipids | |
| Cholesterol | |
| diabetes | |
| Exercise & Physical Activity | |
| Search limits: Not ACP Journal Club OR Summaries for patients OR Editorial OR case-report OR letter OR letter OR abstract OR newspaper article OR comment OR baseline characteristics OR study design OR methodologyTerms to identify clinical trials/SRs/Mas:Filters: Meta-Analysis, Systematic Reviews, Clinical Trial, Controlled Clinical Trial, Randomized Controlled Trial, From 2011/01/01 to 2018/05/25, Humans, English, Adult: 19+ years Terms to identify observational studies:2011/01/01 to 2018/12/31, Humans, English, Epidemiologic Studies, Case-Control Studies, Cohort Studies, Cross-Sectional Studies, epidemiolog* AND stud*, case control, cohort stud*, cross sectional, cohort analys*, follow up stud*, longitudinal, retrospective, prospective, observational AND stud*Filters: Adult: 19+ years | |
| Waist Circumference | |
| Search limited to adult populations, 01/01/201010/3/18, English language | |
| Acute Coronary Syndrome | Acute coronary syndromes |
| Angina Unstable | Unstable angina?, Angina Unstable |
| Myocardial infarction | Myocardial infarctions |
| Shock cardiogenic | shock cardiogenic |
| Myocardial Stunning | myocardial stunning |
| No Reflow Phenomenon | |
| Heart Arrest | |
| St elevation myocardial infarction | STEMI |
| Non-st elevated myocardial | NSTEMI |
| infarction | |
| death/sudden cardiac | |
| Stroke | |
| Brain Infarction | |
| Brain Stem Infarctions | |
| Lateral Meduallary Syndrome | |
| Cerebral Infarction | |
| Myocardial ischemia | |
| Dementia Multi infarct | |
| infarction anterior cerebral artery | |
| infarction middle cerebral artery | |
| infarction posterior cerebral artery | |
| Myocardial revascularization | |
| Coronary artery bypass | |
| Internal mammary coronary artery anastomosis | |
| Angioplasty | angioplasty transluminal percutaneous coronary |
| Heart failure | |
| Hospitalization | Hospitalization? OR rehospitalization? |
| atherectomy coronary | |
| Coronary stent | |
| CABG | |
| bypass grafts | |
| Carotid | |
| pathology | |
| physiopathology | |
| Non-coronary revascularization procedure | |
| Carotid revascularization? | |
| Lower extremity revascularization? | |
| Percutaneous transluminal angioplast? | |
| Stent placement? | |
| Abdominal aortic aneurysm repair? | |
| AAA repair? | |
| complications | |
| Event? OR outcome? OR episode? | |
| Risk score | |
| Coronary risk modification | |
| Cardiovascular diseases | Cardiovascular OR CVD |
| Cardiovascular disease | |
| Coronary disease | coronary |
| Coronary artery disease | |
| Myocardial infarction | |
| Heart failure | CHFORCHD |
| Cerebrovascular disorders | |
| dyspnea paroxysmal | |
| edema cardiac | |
| Physical fitness | |
| Motor activity | |
| Exercise tolerance | |
| Metabolic equivalent | Metabolic equivalent |
| Exercise test | Graded exercise test OR gxt |
| Life style or lifestyle | |
| Exercise | |
| Training | |
| Walking | |
| Vo2 | |
| Maximal met | |
| Mets | |
| Physical activity | |
| Maximal metabolic? | |
| Acute Coronary Syndrome | Acute coronary syndromes |
| Angina Unstable | Unstable angina?, Angina Unstable |
| Myocardial infarction | Myocardial infarctions |
| Shock cardiogenic | shock cardiogenic |
| Myocardial Stunning | myocardial stunning |
| No Reflow Phenomenon | |
| Heart Arrest | |
| St elevation myocardial infarction | STEMI |
| Non-st elevated myocardial infarction | NSTEMI |
| death/sudden cardiac | |
| Stroke | |
| Brain Infarction | |
| Brain Stem Infarctions | |
| Lateral Meduallary Syndrome | |
| Cerebral Infarction | |
| Myocardial ischemia | |
| Dementia Multi infarct | |
| infarction anterior cerebral artery | |
| infarction middle cerebral artery | |
| infarction posterior cerebral artery | |
| Myocardial revascularization | |
| Coronary artery bypass | |
| Internal mammary coronary artery anastomosis | |
| Angioplasty | angioplasty transluminal percutaneous coronary |
| Heart failure | |
| Hospitalization | Hospitalization? OR rehospitalization? |
| atherectomy coronary | |
| Coronary stent | |
| CABG | |
| bypass grafts | |
| Carotid | |
| pathology | |
| physiopathology | |
| Non-coronary revascularization procedure | |
| Carotid revascularization? | |
| Lower extremity revascularization? | |
| Percutaneous transluminal angioplast? | |
| Stent placement? | |
| Abdominal aortic aneurysm repair? | |
| AAA repair? | |
| complications | |
| Event? OR outcome? OR episode? | |
| Risk score | |
| Coronary risk modification | |
| Cardiovascular diseases | Cardiovascular OR CVD |
| Cardiovascular disease | |
| Coronary disease | coronary |
| Coronary artery disease | |
| Myocardial infarction | |
| Heart failure | CHFORCHD |
| Cerebrovascular disorders | |
| dyspnea paroxysmal | |
| edema cardiac |
1.
Patnode CD, Evans CV, Senger CA, et al. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults without known cardiovascular disease risk factors: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2017;318:17593. [PubMed] [Google Scholar]2.
LeBlanc ES, Patnode CD, Webber EM, et al. Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2018;320:117291. [PubMed] [Google Scholar]3.
Selph S, Dana T, Bougatsos C, et al. Screening for abnormal glucose and type 2 diabetes mellitus: a systematic review to update the 2008 U.S. Preventive Services Task Force Recommendation. Report No. 1305190-EF-1.Rockville, MD: U.S. Agency for Healthcare Research and Quality; 2015. Available at: http://www.ncbi.nlm.nih.gov/books/NBK293871. Accessed January 5, 2019. [PubMed] [Google Scholar]4.
Patnode CD, Henderson JT, Thompson JH, et al. Behavioral counseling and pharmacotherapy interventions for tobacco cessation in adults, including pregnant women: a review of reviews for the U.S. Preventive Services Task Force. Ann Intern Med. 2015;163:60821. [PubMed] [Google Scholar]5.
Guirguis-Blake JM, Evans CV, Senger CA, et al. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2016;164:80413. [PubMed] [Google Scholar]Appendix 2.
Author Relationships With Industry and Other Entities (Relevant)2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease
| Committee Member | Employment | Consultant | Speakers Bureau | Ownership/ Partnership/ Principal | Personal Research | Institutional, Organizational, or Other Financial Benefit | Expert Witness |
|---|---|---|---|---|---|---|---|
| Donna K. Arnett (Co-Chair) | University of Kentucky College of Public HealthDean and Professor of Epidemiology | None | None | None | None | None | None |
| Roger S. Blumenthal ( Co-Chair) | Johns Hopkins University Professor of Medicine and Director, Ciccarone Center for the Prevention of Heart Disease | None | None | None | None | None | None |
| Michelle A. Albert | UCSF School of Medicine Professor of Medicine and Director, UCSF NURTURE Center | None | None | None | None | None | None |
| Andrew B. Buroker | Faegre Baker Daniels LLP, Partner | None | , None | None | None | None | None |
| Zachary D. Goldberger | University of Wisconsin School of Medicine and Public Health Associate Professor of Medicine, Division of Cardiology | None | None | None | None | None | None |
| Ellen J. Hahn | University of Kentucky College of NursingProfessor & Director, BREATHE, Deputy Director, UK-CARES & Leader, and Community Engagement Core; Marcia A. Dake Professor of Nursing | None | None | None | None | None | None |
| Cheryl D. Himmelfarb | Johns Hopkins School of NursingProfessor; Associate Dean Research, Office for Science and Innovation; and Deputy Director, Johns Hopkins Institute for Clinical and Translational Research | None | None | None | None | None | None |
| Amit Khera | UT Southwestern School of MedicineProfessor of Internal Medicine and Director, Preventive Cardiology Program | None | None | None | None | None | None |
| Donald Lloyd-Jones | Northwestern UniversityEileen M. Foell Professor; Senior Associate Dean for Clinical and Translational Research; Chair, Department of Preventive Medicine; and Director, Clinical and Translational Sciences Institute | None | None | None | None | None | None |
| J. William McEvoy | National University of Ireland, Galway CampusProfessor of Preventive Cardiology; National Institute for Preventive Cardiology, GalwayMedical and Research Director; and University Hospital Galway, Ireland Consultant Cardiologist. | None | None | None | None | None | None |
| Erin D. Michos | Johns Hopkins School of MedicineAssociate Professor of Medicine and Associate Director of Preventive Cardiology, Ciccarone Center for the Prevention of Heart Disease; Johns Hopkins Bloomberg School of Public HealthAssociate Professor of Epidemiology | None | None | None | None | None | None |
| Michael D. Miedema | Minneapolis Heart Institute Director of Cardiovascular Prevention | None | None | None | None | None | None |
| Daniel Muoz | Vanderbilt University Medical CenterAssistant Professor of Medicine, Division of Cardiology, Medical Director for Quality, Vanderbilt Heart & Vascular Institute, and Associate Medical Director, Cardiovascular ICU | None | None | None | None | None | None |
| Sidney C. Smith, Jr | University of North Carolina, Chapel HillProfessor of Medicine, Division of Cardiology | None | None | None | None | None | None |
| Salim S. Virani | Baylor College of Medicine Professor, Section of Cardiovascular Research and Director for Research, Cardiology Fellowship Training Program; Michael E. DeBakey VA Medical CenterStaff Cardiologist and Investigator, Health Policy, Quality & Informatics Program, Center for Innovations in Quality, Effectiveness and Safety | None | None | None | None | None | None |
| Kim A. Williams, Sr | Rush Medical CollegeJames B. Herrick Professor and Chief, Division of Cardiology, Department of Internal Medicine | None | None | None | None | None | None |
| Joseph Yeboah | Wake Forest Baptist Health Associate Professor, Internal Medicine, Cardiovascular | None | None | None | None | None | None |
| Boback Ziaeian | University of California at Los Angeles, David Geffen School of MedicineClinical Instructor, Division of Cardiology | None | None | None | None | None | None |
Appendix 3.
Reviewer Relationships With Industry and Other Entities (Comprehensive)2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease
| Reviewer | Representation | Employment | Consultant | Speakers Bureau | Ownership/Partnership/Principal | Personal Research | Institutional, Organizational, or Other Financial Benefit | Expert Witness | Salary |
|---|---|---|---|---|---|---|---|---|---|
| Amy Peterson | Official ReviewerAHA | Hospital Affiliations: American Family Childrens Hospital; UnityPoint HealthMeriter; UW School of Medicine and Public Health Department of Pediatrics | None | None | None | None | None | None | None |
| Kim K. Birtcher | Official ReviewerACC/AHA Task Force on Clinical Practice Guidelines Lead Reviewer | University of Houston, College of Pharmacy, Clinical Professor | Jones & Bartlett, Learning | None | None | None | Accreditation Council for Clinical Lipidology (Other category) | None | None |
| Sanjay Gandhi | Official ReviewerACC | Metro Health Medical Center Cleveland, Associate Professor, Case Western Reserve University School of Medicine | None | None | None | Cleveland Heart Lab Juventas | Athersys (Data Safety Monitoring Board) Tendyne(Other category) | None | None |
| Andrea Price | Official ReviewerACC Science and Quality Committee | Quality Databases at Indiana University Health, Director | None | None | None | None | ACC* | None | None |
| Jennifer E. Sanner Beauchamp | Content ReviewerAHA | University of Texas Health Science Center, Cizik School of Nursing, Associate Professor | None | None | None | None | None | None | None |
| Glenn N. Levine | Content ReviewerACC/AHA Task Force on Clinical Practice Guidelines | Professor of Medicine at Baylor College of Medicine in Houston, Texas | None | None | None | None | None | Out of hospital cardiopulmonary arrest 2017 (Defendant)* Out of hospital death 2018 (Defendant)* | None |
| Patrick T. OGara | Content ReviewerACC/AHA Task Force on Clinical Practice Guidelines | Director of Strategic Planning for the Cardiovascular Division at Brigham and Womens Hospital, the Watkins Family Distinguished Chair in Cardiology and Professor of Medicine at Harvard Medical School | None | None | None | None | Edwards Scientific (Other) Medtronic (Other) NIH (Other)* | None | None |
| Joshua A. Beckman | Content ReviewerACC/AHA Task Force on Clinical Practice Guidelines | Director, Vascular Medicine; Professor of Medicine at Vanderbilt University | Aralez Pharmaceuticals* Astra Zeneca Pharmaceuticals* Janssen Scientific Affairs* ER Squibb & Sons Boehringer Ingelheim Pharmaceuticals* Merck Sanofi | AstraZeneca Pharmaceuticals | None | Bristol-Myers Squibb* | Bayer (Data Safety Monitoring Board)* Novartis Corporation (Data Safety Monitoring Board) Vascular Interventional Advances (Officer, Director, Trustee, or other Fiduciary Role)* EMX JanaCare | None | None |
| Anita Deswal | Content ReviewerACC/AHA Task Force on Clinical Practice Guidelines | Chief, Cardiology, Michael E. DeBakey VA Medical Center & Baylor College of Medicine, Professor, Baylor College of Medicine | None | None | None | NIH* | ACC/AHA (Other) Novartis Corporation (Other) AHA Get With The Guidelines Steering Committee (Other) Heart Failure Society of America (Other) Immediate Past Chair and Member, AHA Committee on Heart Failure andTransplantation(Other) NIH (Other) | None | None |
| Federico Gentile | Content ReviewerACC/AHA Task Force on Clinical Practice Guidelines | Centro Medico DiagnosticoDirector, Cardiovascular Disease | None | None | None | None | None | None | None |
| Jos A. Joglar | Content ReviewerACC/AHA Task Force on Clinical Practice Guidelines | Program Director, Clinical CardiacElectrophysiology Fellowship Program; Professor, UT Southwestern Medical Center | None | None | None | None | None | None | None |
| Duminda N. Wijeysundera | Content ReviewerACC/AHA Task Force on Clinical Practice Guidelines | Associate Professor Anesthesia, University of Toronto | None | None | None | Canadian Institutes of Health Research* Ministry of Health and Longterm Care of Ontario (Canada)* NIH* | PCORI (Data Safety Monitoring Board) | None | Canadian Institutes of Health Research (Ottawa, Ontario, Canada)* |
| Eileen M. Handberg | Content ReviewerACC | Research Professor of Medicine; Director, Clinical Trials Program; Program Director, Florida CARES, UF Health | Bristol-Myers Squibb Company | None | None | Aastrom Biosciences* Amorcyte, Inc* Biocardia, Inc* Brigham and Womens Hospital* Capricor* Cytori Therapeutics, Inc* Department of Defense* Direct Flow Medical* Duke Clinical Research Institute* East Carolina University* Everyfit Inc* MEDTRONIC* Merck & Co.,. Inc.* Mesoblast Inc* NIH* PCORI* Sanofi Aventis* | Amgen (Other) AstraZeneca (Other) Boehringer Ingelheim (Other) Daiichi Sankyo (Other) Gilead Sciences, Inc. (Other) Ionis (Other) Relypsa (Other) | None | None |
| Prem Soman | Content ReviewerACC | Associate Professor of Medicine (Cardiology), Director, Nuclear Cardiology, UPMC | Alnylam Pharma | None | American Society of Nuclear Cardiology* | Astellas Pharma US* | None | None | None |
| Eric Stecker | Content ReviewerACC | Associate Professor of Medicine, Division of Cardiovascular Medicine School of Medicine, OHSU | None | None | Hygeia / Desi MD* | American HeartAssociation* Medical Research Foundation of Oregon* | None | None | None |
| PamelaMorris | ContentReviewerACC | Professor, Medical University of South Carolina | Amgen Inc. Sanofi Regeneron | None | None | None | None | None | None |
| Andrew Freeman | Content ReviewerACC | Director, Clinical Cardiology and Operations; Co-Director, Nuclear Cardiology, National Jewish Health | None | Boehringer Ingelheim* | None | None | None | None | None |
| Carl J. Lavie | Content ReviewerACC | Medical Director, Cardiac Rehabilitation and Prevention, Ochsner Clinic Foundation | None | Amgen* ER Squibb & Sons Pfizer* Aralez Pharmaceuticals Amarin Pharma Sanofi Aventis* | None | None | rNone | None | None |
| James Stein | ContentReviewerACC | Director, UW Health Preventive Cardiology Program, Robert Turell Professor in Cardiovascular Research, UW School of Medicine and Public Health | Eli Lilly and Company (DSMB) | None | None | None | Up To Date (Other) Wisconsin Alumni Research Foundation (Other) | None | None |
| HeatherJohnson | ContentReviewerACC | Associate Professor in the Division of Cardiovascular Medicine at the University of Wisconsin School of Medicine and Public Health | None | None | None | None | Pfizer | None | None |
| Nanette Wenger | Content ReviewerACC | Professor of Medicine, Division of Cardiology, Emory University School of Medicine | Janssen Pharmaceuticals, Inc* Amgen AstraZeneca Gilead Sciences Merck | None | None | Gilead Sciences* NHLBI* Pfizer* Society for Womens Health Research* | None | None | None |
| Michael Blaha | ContentReviewerAHA | Director of Clinical Research, Ciccarone Center for the Prevention of Heart Disease Associate Professor of Medicine, Johns Hopkins Medicine | Ferring Pharmaceuticals Regeneron Pharmaceuticals Sanofi-Aventis* Amgen Akcea MedImmune Novartis Novo Nordisk Siemens* ACC | None | None | Aetna Amgen AHA FDA NIH | None | None | None |
| Laurence Sperling | Content ReviewerACC/AHA | Founder and Director of Preventive Cardiology at the Emory Clinic, Co-Director of the Cardiovascular Disease Fellowship Program at Emory, Professor of Medicine (Cardiology) at the Emory University School of Medicine | None | None | None | None | None | None | None |
| Seth Martin | Content ReviewerACC/AHA | Director, Advanced Lipid Disorders Program of the Ciccarone Center; Associate Professor of Medicine at Johns Hopkins Medicine | Amgen Akcea Therapeutics Quest Diagnostics Sanofi-Regeneron Esperion Novo Nordisk | None | None | Aetna Foundation* Apple* Google* iHealth* Maryland Innovation Initiative* AHA* | Corrie Health (Officer, Director, Trustee, or other Fiduciary Role) Co-inventor on pending patent filed by Johns Hopkins University for method of LDL-C estimation (Other) | None | None |
| Samia Mora | Content ReviewerACC/AHA | Associate Professor of Medicine, HarvardMedicine School Director, Center for Lipid Metabolomics, Brigham and Women's Hospital | Pri-Med* Pfizer Quest Diagnostics | None | None | None | C3 Conference (Other) European Atherosclerosis Society (Other) FEBS Congress (Other) Oregon Health & Science University (Other) Vascular BiologyWorking GroupMeeting(Other) Atherotech Diagnostics* Pfizer* Quest Diagnostics* NHLBI* NIDDK* | None | None |
| Clyde Yancy | ContentReviewerACC/AHA | Chief ofCardiology in the Department of Medicine, Northwestern Medicine | None | None | None | None | JAMA Cardiology (Other)* | None | None |
| Quinn Pack | AACVPR | Assistant Professor of Medicine at University of Massachusetts Medical School | None | None | None | None | None | None | None |
| Frank Sacks | ASN | Professor of Cardiovascular Disease Prevention, Harvard School of Public Health | Amgen Pfizer* AstraZeneca* | None | None | None | None | None | None |
| SalvatoreLacagnina | ACPM | System Medical Director of Wellness & Employee Health, Lee Health | None | None | None | None | None | None | None |
| Ron Blankstein | ASPC | Co-Director,CardiovascularImaging TrainingProgram,AssociatePhysician,PreventiveCardiology,Director, CardiacComputedTomography,Brigham Health,AssociateProfessor inMedicine andRadiology,Harvard MedicalSchool | Ekos Corporation Amgen | None | None | Amgen Astellas Sanofi-Aventis | American Society of Nuclear Cardiology (Officer, Director, Trustee, or other Fiduciary Role) Intersocietal Accreditation Commission for Computed Tomography (Officer, Director, Trustee, or other Fiduciary Role) Society of Cardiovascular Computed Tomography (Officer, Director, Trustee, or other Fiduciary Role) | None | None |
| Jo-Ann Eastwood | PCNA | Associate Professor, UCLA School of Nursing | None | None | None | None | None | None | None |
| Stuart Haines | ContentReviewerACC/AHA | Professor of Pharmacy Practice, University of Mississippi | None | None | RxInstructionalSystems* | None | American Association of Colleges of Pharmacy (Officer, Director, Trustee, or other Fiduciary Role) | None | None |
| Michael Rich | AGS | Professor of Medicine, Washington University School of Medicine in St. Louis | None | None | None | None | None | None | None |
Footnotes
This document was approved by the American College of Cardiology Clinical Policy Approval Committee, the American Heart Association Science Advisory and Coordinating Committee, and the American Heart Association Executive Committee in February 2019.
Supplemental materials are available with this article at https://www.ahajournals.org/doi/suppl/10.1161/CIR.0000000000000677
Contributor Information
Donna K. Arnett, University of Kentucky College of Public HealthDean and Professor of Epidemiology.
Roger S. Blumenthal, Johns Hopkins UniversityProfessor of Medicine and Director, Ciccarone Center for the Prevention of Heart Disease.
Michelle A. Albert, UCSF School of MedicineProfessor of Medicine and Director, UCSF NURTURE Center.
Erin D. Michos, Johns Hopkins School of MedicineAssociate Professor of Medicine and Associate Director of Preventive Cardiology, Ciccarone Center for the Prevention of Heart Disease; Johns Hopkins Bloomberg School of Public HealthAssociate Professor of Epidemiology.
Andrew B. Buroker, Faegre Baker Daniels LLP, Partner.
Michael D. Miedema, Minneapolis Heart InstituteDirector of Cardiovascular Prevention.
Zachary D. Goldberger, University of Wisconsin School of Medicine and Public HealthAssociate Professor of Medicine, Division of Cardiology.
Daniel Muoz, Vanderbilt University Medical CenterAssistant Professor of Medicine, Division of Cardiology, Medical Director for Quality, Vanderbilt Heart & Vascular Institute, and Associate Medical Director, Cardiovascular ICU.
Ellen J. Hahn, University of Kentucky College of NursingProfessor & Director, BREATHE, Deputy Director, UKCARES & Leader, and Community Engagement Core; Marcia A. Dake Professor of Nursing.
Sidney C. Smith, Jr, University of North Carolina, Chapel HillProfessor of Medicine, Division of Cardiology.
Cheryl D. Himmelfarb, Johns Hopkins School of NursingProfessor; Associate Dean Research, Office for Science and Innovation; and Deputy Director, Johns Hopkins Institute for Clinical and Translational Research.
Salim S. Virani, Baylor College of MedicineProfessor, Section of Cardiovascular Research and Director for Research, Cardiology Fellowship Training Program; Michael E. DeBakey VA Medical CenterStaff Cardiologist and Investigator, Health Policy, Quality & Informatics Program, Center for Innovations in Quality, Effectiveness and Safety.
Amit Khera, UT Southwestern School of MedicineProfessor of Internal Medicine and Director, Preventive Cardiology Program.
Kim A. Williams, Sr, Rush Medical CollegeJames B. Herrick Professor and Chief, Division of Cardiology, Department of Internal Medicine.
Donald Lloyd-Jones, Northwestern UniversityEileen M. Foell Professor; Senior Associate Dean for Clinical and Translational Research; Chair, Department of Preventive Medicine; and Director, Clinical and Translational Sciences Institute.
Joseph Yeboah, Wake Forest Baptist HealthAssociate Professor, Internal Medicine, Cardiovascular.
J. William McEvoy, National University of Ireland, Galway CampusProfessor of Preventive Cardiology; National Institute for Preventive Cardiology, GalwayMedical and Research Director; and University Hospital Galway, IrelandConsultant Cardiologist.
Boback Ziaeian, University of California at Los Angeles, David Geffen School of MedicineClinical Instructor, Division of Cardiology.
References
1.Introduction
S11.
Weir HK, Anderson RN, Coleman King SM, et al. Heart disease and cancer deathstrends and projections in the United States, 19692020. Prev Chronic Dis. 2016;13:E157. [PMC free article] [PubMed] [Google Scholar]S12.
Johnson NB, Hayes LD, Brown K, et al. CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factorsUnited States, 20052013. MMWR Suppl. 2014;63:327. [PubMed] [Google Scholar]S13.
Xu J, Murphy SL, Kochanek KD, et al. Mortality in the United States, 2015. NCHS Data Brief. 2016;18. [PubMed] [Google Scholar]S14.
Greenland P, Knoll MD, Stamler J, et al. Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA. 2003;290:8917. [PubMed] [Google Scholar]S15.
Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Associations Strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586613. [PubMed] [Google Scholar]S16.
Turco JV, Inal-Veith A, Fuster V. Cardiovascular health promotion: an issue that can no longer wait. J Am Coll Cardiol. 2018;72:90813. [PubMed] [Google Scholar]S17.
Younus A, Aneni EC, Spatz ES, et al. A systematic review of the prevalence and outcomes of ideal cardiovascular health in US and non-US populations. Mayo Clin Proc. 2016;91:64970. [PubMed] [Google Scholar]1.1.Methodology and Evidence Review
S1.11.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13115. [PubMed] [Google Scholar]S1.12.
Grundy SM, Stone NJ, Bailey AL, et al. 2018. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published online ahead of print November 10, 2018]. Circulation. doi: 10.1161/CIR.0000000000000625 [PubMed] [CrossRef] [Google Scholar]1.5.Class of Recommendation and Level of Evidence
S1.51.
Halperin JL, Levine GN, Al-Khatib SM, et al. Further evolution of the ACC/AHA clinical practice guideline recommendation classification system: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2016;133:14268. [PubMed] [Google Scholar]2.1.Patient-Centered Approaches for Providing Comprehensive ASCVD Prevention
S2.11.
Carter BL, Rogers M, Daly J, et al. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med. 2009;169:174855. [PMC free article] [PubMed] [Google Scholar]S2.12.
Chisholm-Burns MA, Kim Lee J, Spivey CA, et al. US pharmacists effect as team members on patient care: systematic review and meta-analyses. Med Care. 2010;48:92333. [PubMed] [Google Scholar]S2.13.
Fazel MT, Bagalagel A, Lee JK, et al. Impact of diabetes care by pharmacists as part of health care team in ambulatory settings: a systematic review and meta-analysis. Ann Pharmacother. 2017;51:890907. [PubMed] [Google Scholar]S2.14.
Mills KT, Obst KM, Shen W, et al. Comparative effectiveness of implementation strategies for blood pressure control in hypertensive patients: a systematic review and meta-analysis. Ann Intern Med. 2018;168:11020. [PMC free article] [PubMed] [Google Scholar]S2.15.
Proia KK, Thota AB, Njie GJ, et al. Team-based care and improved blood pressure control: a community guide systematic review. Am J Prev Med. 2014;47:8699. [PMC free article] [PubMed] [Google Scholar]S2.16.
Chen Z, Ernst ME, Ardery G, et al. Physician-pharmacist co-management and 24-hour blood pressure control. J Clin Hypertens (Greenwich). 2013;15:33743. [PMC free article] [PubMed] [Google Scholar]S2.17.
Hirsch JD, Steers N, Adler DS, et al. Primary care-based, pharmacist-physician collaborative medication-therapy management of hypertension: a randomized, pragmatic trial. Clin Ther. 2014;36:124454. [PMC free article] [PubMed] [Google Scholar]S2.18.
Hunt JS, Siemienczuk J, Pape G, et al. A randomized controlled trial of team-based care: impact of physician-pharmacist collaboration on uncontrolled hypertension. J Gen Intern Med. 2008;23:196672. [PMC free article] [PubMed] [Google Scholar]S2.19.
Isetts BJ, Buffington DE, Carter BL, et al. Evaluation of pharmacists work in a physician-pharmacist collaborative model for the management of hypertension. Pharmacotherapy. 2016;36:37484. [PMC free article] [PubMed] [Google Scholar]S2.110.
McLean DL, McAlister FA, Johnson JA, et al. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: study of cardiovascular risk intervention by pharmacists-hypertension (SCRIP-HTN). Arch Intern Med. 2008;168:235561. [PubMed] [Google Scholar]S2.111.
Polgreen LA, Han J, Carter BL, et al. Cost-effectiveness of a physician-pharmacist collaboration intervention to improve blood pressure control. Hypertension. 2015;66:114551. [PMC free article] [PubMed] [Google Scholar]S2.112.
Chen EH, Thom DH, Hessler DM, et al. Using the Teamlet Model to improve chronic care in an academic primary care practice. J Gen Intern Med. 2010;25(suppl 4):S6104. [PMC free article] [PubMed] [Google Scholar]S2.113.
Kravetz JD, Walsh RF. Team-based hypertension management to improve blood pressure control. J Prim Care Community Health. 2016;7:2725. [PMC free article] [PubMed] [Google Scholar]S2.114.
Wan EYF, Fung CSC, Jiao27 FF, et al. Five-year effectiveness of the Multidisciplinary Risk Assessment and Management Programme-Diabetes Mellitus (RAMP-DM) on diabetes-related complications and health service usesa population-based and propensity-matched cohort study. Diabetes Care. 2018;41:4959. [PubMed] [Google Scholar]S2.115.
Buhse S, Mhlhauser I, Heller T, et al. Informed shared decision-making programme on the prevention of myocardial infarction in type 2 diabetes: a randomised controlled trial. BMJ Open. 2015;5:e009116. [PMC free article] [PubMed] [Google Scholar]S2.116.
Cooper LA, Roter DL, Carson KA, et al. A randomized trial to improve patient-centered care and hypertension control in underserved primary care patients. J Gen Intern Med. 2011;26:1297304. [PMC free article] [PubMed] [Google Scholar]S2.117.
Olomu A, Hart-Davidson W, Luo Z, et al. Implementing shared decision making in federally qualified health centers, a quasi-experimental design study: the Office-Guidelines Applied to Practice (Office-GAP) program. BMC Health S24erv Res. 2016;16:334. [PMC free article] [PubMed] [Google Scholar]S2.118.
Parchman ML, Zeber JE, Palmer RF. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann Fam Med. 2010;8:4107. [PMC free article] [PubMed] [Google Scholar]S2.119.
Havranek EP, Mujahid MS, Barr DA, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:87398. [PubMed] [Google Scholar]S2.120.
Vilhelmsson A, stergren P-O. Reducing health inequalities with interventions targeting behavioral factors among individuals with low levels of educationa rapid review. PLoS ONE. 2018;13:e0195774. [PMC free article] [PubMed] [Google Scholar]S2.121.
Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. 2018;137:216678. [PMC free article] [PubMed] [Google Scholar]S2.122.
Backholer K, Peters SAE, Bots SH, et al. Sex differences in the relationship between socioeconomic status and cardiovascular disease: a systematic review and meta-analysis. J Epidemiol Community Health. 2017;71:5507. [PubMed] [Google Scholar]S2.123.
Beauchamp A, Peeters A, Tonkin A, et al. Best practice for prevention and treatment of cardiovascular disease through an equity lens: a review. Eur J Cardiovasc Prev Rehabil. 2010;17:599606. [PubMed] [Google Scholar]S2.124.
Khaing W, Vallibhakara SA, Attia J, et al. Effects of education and income on cardiovascular outcomes: a systematic review and meta-analysis. Eur J Prev Cardiol. 2017;24:103242. [PubMed] [Google Scholar]S2.125.
Pollitt RA, Rose KM, Kaufman JS. Evaluating the evidence for models of life course socioeconomic factors and cardiovascular outcomes: a systematic review. BMC Public Health. 2005;5:7. [PMC free article] [PubMed] [Google Scholar]S2.126.
DeFilippis AP, Young R, McEvoy JW, et al. Risk score overestimation: the impact of individual cardiovascular risk factors and preventive therapies on the performance of the American Heart Association-American College of Cardiology-Atherosclerotic Cardiovascular Disease risk score in a modern multi-ethnic cohort. Eur Heart J. 2017;38:598608. [PMC free article] [PubMed] [Google Scholar]S2.127.
Magnani JW, Mujahid MS, Aronow HD, et al. Health literacy and cardiovascular disease: fundamental relevance to primary and secondary prevention: a scientific statement from the American Heart Association. Circulation. 2018;138:e4874. [PMC free article] [PubMed] [Google Scholar]S2.128.
Powell TM, de Lemos JA, Banks K, et al. Body size misperception: a novel determinant in the obesity epidemic. Arch Intern Med. 2010;170:16957. [PMC free article] [PubMed] [Google Scholar]S2.129.
Padgett J, Biro FM. Different shapes in different cultures: body dissatisfaction, overweight, and obesity in African-American and caucasian females. J Pediatr Adolesc Gynecol. 2003;16:34954. [PubMed] [Google Scholar]S2.131.
Malambo P, Kengne AP, De Villiers A, et al. Built environment, selected risk factors and major cardiovascular disease outcomes: a systematic review. PLoS ONE. 2016;11:e0166846. [PMC free article] [PubMed] [Google Scholar]S2.132.
Bird EL, Ige JO, Pilkington P, et al. Built and natural environment planning principles for promoting health: an umbrella review. BMC Public Health. 2018;18:930. [PMC free article] [PubMed] [Google Scholar]S2.133.
Kaiser P, Diez Roux AV, Mujahid M, et al. Neighborhood environments and incident hypertension in the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2016;183:98897. [PMC free article] [PubMed] [Google Scholar]S2.134.
Kumanyika SK, Gary TL, Lancaster KJ, et al. Achieving healthy weight in African-American communities: research perspectives and priorities. Obes Res. 2005;13:203747. [PubMed] [Google Scholar]S2.135.
Grandner MA. Addressing sleep disturbances: an opportunity to prevent cardiometabolic disease?Int Rev Psychiatry. 2014;26:15576. [PMC free article] [PubMed] [Google Scholar]S2.136.
Knutson KL. Sociodemographic and cultural determinants of sleep deficiency: implications for cardiometabolic disease risk. Soc Sci Med. 2013;79:715. [PMC free article] [PubMed] [Google Scholar]S2.137.
Ismail K, Winkley K, Rabe-Hesketh S. Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Lancet. 2004;363:158997. [PubMed] [Google Scholar]S2.138.
Alam R, Sturt J, Lall R, et al. An updated meta-analysis to assess the effectiveness of psychological interventions delivered by psychological specialists and generalist clinicians on glycaemic control and on psychological status. Patient Educ Couns. 2009;75:2536. [PubMed] [Google Scholar]S2.139.
Bolen SD, Chandar A, Falck-Ytter C, et al. Effectiveness and safety of patient activation interventions for adults with type 2 diabetes: systematic review, meta-analysis, and meta-regression. J Gen Intern Med. 2014;29:116676. [PMC free article] [PubMed] [Google Scholar]S2.140.
Gonzalez JS, Tanenbaum ML, Commissariat PV. Psychosocial factors in medication adherence and diabetes self-management: Implications for research and practice. Am Psychol. 2016;71:53951. [PMC free article] [PubMed] [Google Scholar]S2.142.
Samuel LJ, Dennison Himmelfarb CR, Szklo M, et al. Social engagement and chronic disease risk behaviors: the Multi-Ethnic Study of Atherosclerosis. Prev Med. 2015;71:616. [PMC free article] [PubMed] [Google Scholar]S2.143.
Verbiest M, Brakema E, van der Kleij R, et al. National guidelines for smoking cessation in primary care: a literature review and evidence analysis. NPJ Prim Care Respir Med. 2017;27:2. [PMC free article] [PubMed] [Google Scholar]2.2.Assessment of Cardiovascular Risk
S2.21.
Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:293559. [PMC free article] [PubMed] [Google Scholar]S2.23.
Ference BA, Graham I, Tokgozoglu L, et al. Impact of lipids on cardiovascular health: JACC Health Promotion Series. J Am Coll Cardiol. 2018;72:114156. [PubMed] [Google Scholar]S2.24.
Grundy SM, Stone NJ, Bailey AL, et al. 2018. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published online ahead of print November 10, 2018]. Circulation. doi: 10.1161/CIR.0000000000000625 [PubMed] [CrossRef] [Google Scholar]S2.25.
Patel J, Al Rifai M, Scheuner MT, et al. Basic vs more complex definitions of family history in the prediction of coronary heart disease: the Multi-Ethnic Study of Atherosclerosis. Mayo Clin Proc. 2018;93:121323. [PMC free article] [PubMed] [Google Scholar]S2.26.
del Rincn ID, Williams K, Stern MP, et al. High incidence of cardiovascular events in a rheumatoid arthritis cohort not explained by traditional cardiac risk factors. Arthritis Rheum. 2001;44:273745. [PubMed] [Google Scholar]S2.27.
Manzi S, Meilahn EN, Rairie JE, et al. Age-specific incidence rates of myocardial infarction and angina in women with systemic lupus erythematosus: comparison with the Framingham Study. Am J Epidemiol. 1997;145:40815. [PubMed] [Google Scholar]S2.28.
Wu P, Haththotuwa R, Kwok CS, et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2017;10:e003497. [PubMed] [Google Scholar]S2.29.
Tanz LJ, Stuart JJ, Williams PL, et al. Preterm delivery and maternal cardiovascular disease in young and middle-aged adult women. Circulation. 2017;135:57889. [PMC free article] [PubMed] [Google Scholar]S2.210.
Wellons M, Ouyang P, Schreiner PJ, et al. Early menopause predicts future coronary heart disease and stroke: the Multi-Ethnic Study of Atherosclerosis. Menopause. 2012;19:10817. [PMC free article] [PubMed] [Google Scholar]S2.211.
Uddin SMI, Mirbolouk M, Dardari Z, et al. Erectile dysfunction as an independent predictor of future cardiovascular events. Circulation. 2018;138:5402. [PMC free article] [PubMed] [Google Scholar]S2.212.
Triant VA, Perez J, Regan S, et al. Cardiovascular risk prediction functions underestimate risk in HIV infection. Circulation. 2018;137:220314. [PMC free article] [PubMed] [Google Scholar]S2.213.
Volgman AS, Palaniappan LS, Aggarwal NT, et al. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation. 2018;138:e134. [PubMed] [Google Scholar]S2.214.
Ridker PM, Danielson E, Fonseca FAH, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195207. [PubMed] [Google Scholar]S2.215.
DeFilippis AP, Young R, Carrubba CJ, et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med. 2015;162:26675. [PMC free article] [PubMed] [Google Scholar]S2.216.
Mahabadi AA, Mhlenkamp S, Lehmann N, et al. CAC score improves coronary and CV risk assessment above statin indication by ESC and AHA/ACC primary prevention guidelines. JACC Cardiovasc Imaging. 2017;10:14353. [PubMed] [Google Scholar]S2.217.
Budoff MJ, Young R, Burke G, et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: the Multi-Ethnic Study of Atherosclerosis (MESA). Eur Heart J. 2018;39:24018. [PMC free article] [PubMed] [Google Scholar]S2.218.
McClelland RL, Jorgensen NW, Budoff M, et al. 10-year coronary heart disease risk prediction using coronary artery calcium and traditional risk factors: derivation in the MESA (Multi-Ethnic Study of Atherosclerosis) with validation in the HNR (Heinz Nixdorf Recall) study and the DHS (Dallas Heart Study). J Am Coll Cardiol. 2015;66:164353. [PMC free article] [PubMed] [Google Scholar]S2.219.
Kavousi M, Desai CS, Ayers C, et al. Prevalence and prognostic implications of coronary artery calcification in low-risk women: a meta-analysis. JAMA. 2016;316:212634. [PubMed] [Google Scholar]S2.220.
Carr JJ, Jacobs DR Jr, Terry JG, et al. Association of coronary artery calcium in adults aged 32 to 46 years with incident coronary heart disease and death. JAMA Cardiol. 2017;2:3919. [PMC free article] [PubMed] [Google Scholar]S2.221.
Mortensen MB, Fuster V, Muntendam P, et al. A simple disease-guided approach to personalize ACC/AHA-recommended statin allocation in elderly people: the BioImage Study. J Am Coll Cardiol. 2016;68:88191. [PubMed] [Google Scholar]S2.222.
Blaha MJ, Cainzos-Achirica M, Greenland P, et al. Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: The Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2016;133:84958. [PMC free article] [PubMed] [Google Scholar]S2.223.
Patel J, Al Rifai M, Blaha MJ, et al. Coronary artery calcium improves risk assessment in adults with a family history of premature coronary heart disease: results from the Multi-Ethnic Study of Atherosclerosis. Circ Cardiovasc Imaging. 2015;8:e003186. [PMC free article] [PubMed] [Google Scholar]S2.224.
Pursnani A, Massaro JM, DAgostino RB Sr, et al. Guideline-based statin eligibility, coronary artery calcification, and cardiovascular events. JAMA. 2015;314:13441. [PMC free article] [PubMed] [Google Scholar]S2.225.
Valenti V Hartaigh B, Heo R, et al. A 15-year warranty period for asymptomatic individuals without coronary artery calcium: a prospective follow-up of 9,715 individuals. JACC Cardiovasc Imaging. 2015;8:9009. [PMC free article] [PubMed] [Google Scholar]S2.226.
Yano Y, ODonnell CJ, Kuller L, et al. Association of coronary artery calcium score vs age with cardiovascular risk in older adults: an analysis of pooled population-based studies. JAMA Cardiol. 2017;2:98694. [PMC free article] [PubMed] [Google Scholar]S2.227.
Yeboah J, Young R, McClelland RL, et al. Utility of nontraditional risk markers in atherosclerotic cardiovascular disease risk assessment. J Am Coll Cardiol. 2016;67:13947. [PMC free article] [PubMed] [Google Scholar]S2.230.
Gupta A, Lau E, Varshney R, et al. The identification of calcified coronary plaque is associated with initiation and continuation of pharmacological and lifestyle preventive therapies: a systematic review and meta-analysis. JACC Cardiovasc Imaging. 2017;10:83342. [PMC free article] [PubMed] [Google Scholar]S2.231.
Shah RV, Spahillari A, Mwasongwe S, et al. Subclinical atherosclerosis, statin eligibility, and outcomes in African American individuals: the Jackson Heart Study. JAMA Cardiol. 2017;2:64452. [PMC free article] [PubMed] [Google Scholar]S2.232.
Lloyd-Jones DM, Leip EP, Larson MG, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:7918. [PubMed] [Google Scholar]S2.234.
Wilkins JT, Ning H, Berry J, et al. Lifetime risk and years lived free of total cardiovascular disease. JAMA. 2012;308:1795801. [PMC free article] [PubMed] [Google Scholar]S2.235.
Pencina MJ, DAgostino RB Sr, Larson MG, et al. Predicting the 30-year risk of cardiovascular disease: the Framingham Heart Study. Circulation. 2009;119:307884. [PMC free article] [PubMed] [Google Scholar]S2.236.
Nasir K, Bittencourt MS, Blaha MJ, et al. Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association cholesterol management guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2015;66:165768. [PubMed] [Google Scholar]3.1.Nutrition and Diet
S3.11.
Estruch R, Ros E, Salas-Salvad J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018;378:e34. [PubMed] [Google Scholar]S3.12.
Kim H, Caulfield LE, Rebholz CM. Healthy plant-based diets are associated with lower risk of all-cause mortality in US adults. J Nutr. 2018;148:62431. [PMC free article] [PubMed] [Google Scholar]S3.13.
Reedy J, Krebs-Smith SM, Miller PE, et al. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. 2014;144:8819. [PMC free article] [PubMed] [Google Scholar]S3.14.
Satija A, Bhupathiraju SN, Spiegelman D, et al. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in US adults. J Am Coll Cardiol. 2017;70:41122. [PMC free article] [PubMed] [Google Scholar]S3.15.
Sotos-Prieto M, Bhupathiraju SN, Mattei J, et al. Association of changes in diet quality with total and cause-specific mortality. N Engl J Med. 2017;377:14353. [PMC free article] [PubMed] [Google Scholar]S3.16.
Whalen KA, Judd S, McCullough ML, et al. Paleolithic and Mediterranean diet pattern scores are inversely associated with all-cause and cause-specific mortality in adults. J Nutr. 2017;147:61220. [PMC free article] [PubMed] [Google Scholar]S3.17.
Bao Y, Han J, Hu FB, et al. Association of nut consumption with total and cause-specific mortality. N Engl J Med. 2013;369:200111. [PMC free article] [PubMed] [Google Scholar]S3.18.
Bernstein AM, Sun Q, Hu FB, et al. Major dietary protein sources and risk of coronary heart disease in women. Circulation. 2010;122:87683. [PMC free article] [PubMed] [Google Scholar]S3.19.
Song M, Fung TT, Hu FB, et al. Association of animal and plant protein intake with all-cause and cause-specific mortality. JAMA Intern Med. 2016;176:145363. [PMC free article] [PubMed] [Google Scholar]S3.110.
Tharrey M, Mariotti F, Mashchak A, et al. Patterns of plant and animal protein intake are strongly associated with cardiovascular mortality: the Adventist Health Study-2 cohort. Int J Epidemiol. 2018;47:160312. [PMC free article] [PubMed] [Google Scholar]S3.111.
Martnez-Gonzlez MA, Snchez-Tainta A, Corella D, et al. A provegetarian food pattern and reduction in total mortality in the Prevencin con Dieta Mediterrnea (PREDIMED) study. Am J Clin Nutr. 2014;100(suppl 1):320S8S. [PubMed] [Google Scholar]S3.112.
Wang DD, Li Y, Chiuve SE, et al. Association of specific dietary fats with total and cause-specific mortality. JAMA Intern Med. 2016;176:113445. [PMC free article] [PubMed] [Google Scholar]S3.113.
Dehghan M, Mente A, Zhang X, et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017;390:205062. [PubMed] [Google Scholar]S3.114.
Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:310. [PubMed] [Google Scholar]S3.115.
Cook NR, Cutler JA, Obarzanek E, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 2007;334:8858. [PMC free article] [PubMed] [Google Scholar]S3.116.
Micha R, Pealvo JL, Cudhea F, et al. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017;317:91224. [PMC free article] [PubMed] [Google Scholar]S3.117.
Kiage JN, Merrill PD, Robinson CJ, et al. Intake of trans fat and all-cause mortality in the Reasons for Geographical and Racial Differences in Stroke (REGARDS) cohort. Am J Clin Nutr. 2013;97:11218. [PMC free article] [PubMed] [Google Scholar]S3.118.
Lfvenborg JE, Andersson T, Carlsson P-O, et al. Sweetened beverage intake and risk of latent autoimmune diabetes in adults (LADA) and type 2 diabetes. Eur J Endocrinol. 2016;175:60514. [PubMed] [Google Scholar]S3.119.
Yang Q, Zhang Z, Gregg EW, et al. Added sugar intake and cardiovascular diseases mortality among US adults. JAMA Intern Med. 2014;174:51624. [PMC free article] [PubMed] [Google Scholar]S3.120.
Johnson RK, Lichtenstein AH, Anderson CAM, et al. Low-calorie sweetened beverages and cardiometabolic health: a science advisory from the American Heart Association. Circulation. 2018;138:e12640. [PubMed] [Google Scholar]S3.121.
Shikany JM, Safford MM, Newby PK, et al. Southern dietary pattern is associated with hazard of acute coronary heart disease in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study. Circulation. 2015;132:80414. [PMC free article] [PubMed] [Google Scholar]S3.122.
Seidelmann SB, Claggett B, Cheng S, et al. Dietary carbohydrate intake and mortality: a prospective cohort study and meta-analysis. Lancet Public Health. 2018;3:e41928. [PMC free article] [PubMed] [Google Scholar]S3.123.
Trichopoulou A, Psaltopoulou T, Orfanos P, et al. Low-carbohydrate-high-protein diet and long-term survival in a general population cohort. Eur J Clin Nutr. 2007;61:57581. [PubMed] [Google Scholar]S3.124.
Noto H, Goto A, Tsujimoto T, et al. Low-carbohydrate diets and all-cause mortality: a systematic review and meta-analysis of observational studies. PLoS ONE. 2013;8:e55030. [PMC free article] [PubMed] [Google Scholar]S3.125.
Brandt EJ, Myerson R, Perraillon MC, et al. Hospital admissions for myocardial infarction and stroke before and after the trans-fatty acid restrictions in New York. JAMA Cardiol. 2017;2:62734. [PMC free article] [PubMed] [Google Scholar]S3.126.
Micha R, Mozaffarian D. Trans fatty acids: effects on metabolic syndrome, heart disease and diabetes. Nat Rev Endocrinol. 2009;5:33544. [PubMed] [Google Scholar]S3.127.
Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation. 2016;133:187225. [PMC free article] [PubMed] [Google Scholar]3.2.Exercise and Physical Activity
S3.21.
Orrow G, Kinmonth A-L, Sanderson S, et al. Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ. 2012;344:e1389. [PMC free article] [PubMed] [Google Scholar]S3.22.
Sanchez A, Bully P, Martinez C, et al. Effectiveness of physical activity promotion interventions in primary care: a review of reviews. Prev Med. 2015;76(suppl):S5667. [PubMed] [Google Scholar]S3.23.
Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388:130210. [PubMed] [Google Scholar]S3.24.
Hamer M, Chida Y. Walking and primary prevention: a meta-analysis of prospective cohort studies. Br J Sports Med. 2008;42:23843. [PubMed] [Google Scholar]S3.25.
Kyu HH, Bachman VF, Alexander LT, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ. 2016;354:i3857. [PMC free article] [PubMed] [Google Scholar]S3.26.
Sattelmair J, Pertman J, Ding EL, et al. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011;124:78995. [PMC free article] [PubMed] [Google Scholar]S3.27.
Zheng H, Orsini N, Amin J, et al. Quantifying the dose-response of walking in reducing coronary heart disease risk: meta-analysis. Eur J Epidemiol. 2009;24:18192. [PubMed] [Google Scholar]S3.28.
Wahid A, Manek N, Nichols M, et al. Quantifying the association between physical activity and cardiovascular disease and diabetes: a systematic review and meta-analysis. J Am Heart Assoc. 2016;5:e002495. [PMC free article] [PubMed] [Google Scholar]S3.29.
Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162:12332. [PubMed] [Google Scholar]S3.210.
Chomistek AK, Manson JE, Stefanick ML, et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease: results from the Womens Health Initiative. J Am Coll Cardiol. 2013;61:234654. [PMC free article] [PubMed] [Google Scholar]S3.211.
Patterson R, McNamara E, Tainio M, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol. 2018;33:81129. [PMC free article] [PubMed] [Google Scholar]S3.212.
Young DR, Hivert M-F, Alhassan S, et al. Sedentary behavior and cardiovascular morbidity and mortality: a science advisory from the American Heart Association. Circulation. 2016;134:e26279. [PubMed] [Google Scholar]4.1.Obesity and Being Overweight
S4.12.
Ma C, Avenell A, Bolland M, et al. Effects of weight loss interventions for adults who are obese on mortality, cardiovascular disease, and cancer: systematic review and meta-analysis. BMJ. 2017;359:j4849. [PMC free article] [PubMed] [Google Scholar]S4.13.
Canoy D, Cairns BJ, Balkwill A, et al. Coronary heart disease incidence in women by waist circumference within categories of body mass index. Eur J Prev Cardiol. 2013;20:75962. [PubMed] [Google Scholar]S4.14.
Warren TY, Wilcox S, Dowda M, et al. Independent association of waist circumference with hypertension and diabetes in African American women, South Carolina, 20072009. Prev Chronic Dis. 2012;9:E105. [PMC free article] [PubMed] [Google Scholar]S4.15.
Czernichow S, Kengne A-P, Stamatakis E, et al. Body mass index, waist circumference and waist-hip ratio: which is the better discriminator of cardiovascular disease mortality risk?: evidence from an individual-participant meta-analysis of 82 864 participants from nine cohort studies. Obes Rev. 2011;12:6807. [PMC free article] [PubMed] [Google Scholar]S4.16.
Flint AJ, Rexrode KM, Hu FB, et al. Body mass index, waist circumference, and risk of coronary heart disease: a prospective study among men and women. Obes Res Clin Pract. 2010;4:e17181. [PMC free article] [PubMed] [Google Scholar]4.2.Type 2 Diabetes Mellitus
S4.21.
Huo R, Du T, Xu Y, et al. Effects of Mediterranean-style diet on glycemic control, weight loss and cardiovascular risk factors among type 2 diabetes individuals: a meta-analysis. Eur J Clin Nutr. 2015;69:12008. [PubMed] [Google Scholar]S4.22.
Azadbakht L, Fard NRP, Karimi M, et al. Effects of the Dietary Approaches to Stop Hypertension (DASH) eating plan on cardiovascular risks among type 2 diabetic patients: a randomized crossover clinical trial. Diabetes Care. 2011;34:557. [PMC free article] [PubMed] [Google Scholar]S4.23.
Snowling NJ, Hopkins WG. Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis. Diabetes Care. 2006;29:251827. [PubMed] [Google Scholar]S4.24.
Church TS, Blair SN, Cocreham S, et al. Effects of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2010;304:225362. [PMC free article] [PubMed] [Google Scholar]S4.25.
Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:85465. [PubMed] [Google Scholar]S4.26.
Maruthur NM, Tseng E, Hutfless S, et al. Diabetes medications as monotherapy or metformin-based combination therapy for type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med. 2016;164:74051. [PubMed] [Google Scholar]S4.27.
Hong J, Zhang Y, Lai S, et al. Effects of metformin versus glipizide on cardiovascular outcomes in patients with type 2 diabetes and coronary artery disease. Diabetes Care. 2013;36:130411. [PMC free article] [PubMed] [Google Scholar]S4.28.
Griffin SJ, Leaver JK, Irving GJ. Impact of metformin on cardiovascular disease: a meta-analysis of randomised trials among people with type 2 diabetes. Diabetologia. 2017;60:16209. [PMC free article] [PubMed] [Google Scholar]S4.29.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:211728. [PubMed] [Google Scholar]S4.210.
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377:64457. [PubMed] [Google Scholar]S4.211.
Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375:31122. [PMC free article] [PubMed] [Google Scholar]S4.212.
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2018. doi: 10.1056/NEJMoa1812389. [PubMed] [CrossRef] [Google Scholar]S4.213.
Hernandez AF, Green JB, Janmohamed S, et al. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): a double-blind, randomised placebo-controlled trial. Lancet. 2018;392:151929. [PubMed] [Google Scholar]S4.214.
Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375:183444. [PubMed] [Google Scholar]4.3.High Blood Cholesterol
S4.31.
Grundy SM, Stone NJ, Bailey AL, et al. 2018. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published online ahead of print November 10, 2018]. Circulation. doi: 10.1161/CIR.0000000000000625 [PubMed] [CrossRef] [Google Scholar]S4.32.
Cholesterol Treatment Trialists (CTT) Collaboration, Baigent C, Blackwell L, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:167081. [PMC free article] [PubMed] [Google Scholar]S4.33.
Baigent C, Landray MJ, Reith C, et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet. 2011;377:218192. [PMC free article] [PubMed] [Google Scholar]S4.34.
Cholesterol Treatment Trialists (CTT) Collaboration, Herrington W, Emberson J, et al. Impact of renal function on the effects of LDL cholesterol lowering with statin-based regimens: a meta-analysis of individual participant data from 28 randomised trials. Lancet Diabetes Endocrinol. 2016;4:82939. [PubMed] [Google Scholar]S4.35.
Chou R, Dana T, Blazina I, et al. Statin use for the prevention of cardiovascular disease in adults: a systematic review for the U.S. Preventive Services Task Force. Report No. 1405206-EF-2.Rockville, MD: U.S. Agency for Healthcare Research and Quality; 2016. Available at: http://www.ncbi.nlm.nih.gov/books/NBK396415. Accessed January 5, 2019. [PubMed] [Google Scholar]S4.36.
Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279:161522. [PubMed] [Google Scholar]S4.37.
Ridker PM, Danielson E, Fonseca FAH, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195207. [PubMed] [Google Scholar]S4.38.
Taylor F, Huffman MD, Macedo AF, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;CD004816. [PMC free article] [PubMed] [Google Scholar]S4.39.
Yusuf S, Bosch J, Dagenais G, et al. Cholesterol lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374:202131. [PubMed] [Google Scholar]S4.310.
Silverman MG, Ference BA, Im K, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA. 2016;316:128997. [PubMed] [Google Scholar]S4.311.
Colhoun HM, Betteridge DJ, Durrington PN, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet. 2004;364:68596. [PubMed] [Google Scholar]S4.312.
Collins R, Armitage J, Parish S, et al. MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet. 2003;361:200516. [PubMed] [Google Scholar]S4.313.
de Vries FM, Denig P, Pouwels KB, et al. Primary prevention of major cardiovascular and cerebrovascular events with statins in diabetic patients: a meta-analysis. Drugs. 2012;72:236573. [PubMed] [Google Scholar]S4.314.
Knopp RH, dEmden M, Smilde JG, et al. Efficacy and safety of atorvastatin in the prevention of cardiovascular end points in subjects with type 2 diabetes: the Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in non-insulin-dependent diabetes mellitus (ASPEN). Diabetes Care. 2006;29:147885. [PubMed] [Google Scholar]S4.315.
Mulnier HE, Seaman HE, Raleigh VS, et al. Risk of myocardial infarction in men and women with type 2 diabetes in the UK: a cohort study using the General Practice Research Database. Diabetologia. 2008;51:163945. [PubMed] [Google Scholar]S4.316.
Rana JS, Liu JY, Moffet HH, et al. Diabetes and prior coronary heart disease are not necessarily risk equivalent for future coronary heart disease events. J Gen Intern Med. 2016;31:38793. [PMC free article] [PubMed] [Google Scholar]S4.317.
Sever PS, Poulter NR, Dahlf B, et al. Reduction in cardiovascular events with atorvastatin in 2,532 patients with type 2 diabetes: Anglo-Scandinavian Cardiac Outcomes Triallipid-lowering arm (ASCOT-LLA). Diabetes Care. 2005;28:11517. [PubMed] [Google Scholar]S4.318.
Soedamah-Muthu SS, Fuller JH, Mulnier HE, et al. High risk of cardiovascular disease in patients with type 1 diabetes in the U.K.: a cohort study using the general practice research database. Diabetes Care. 2006;29:798804. [PubMed] [Google Scholar]S4.319.
Wong ND, Glovaci D, Wong K, et al. Global cardiovascular disease risk assessment in United States adults with diabetes. Diab Vasc Dis Res. 2012;9:14652. [PubMed] [Google Scholar]S4.320.
Besseling J, Hovingh GK, Huijgen R, et al. Statins in familial hypercholesterolemia: consequences for coronary artery disease and all-cause mortality. J Am Coll Cardiol. 2016;68:25260. [PubMed] [Google Scholar]S4.321.
Khera AV, Won H-H, Peloso GM, et al. Diagnostic yield and clinical utility of sequencing familial hypercholesterolemia genes in patients with severe hypercholesterolemia. J Am Coll Cardiol. 2016;67:257889. [PMC free article] [PubMed] [Google Scholar]S4.322.
Nanchen D, Gencer B, Muller O, et al. Prognosis of patients with familial hypercholesterolemia after acute coronary syndromes. Circulation. 2016;134:698709. [PubMed] [Google Scholar]S4.323.
Perak AM, Ning H, de Ferranti SD, et al. Long-term risk of atherosclerotic cardiovascular disease in US adults with the familial hypercholesterolemia phenotype. Circulation. 2016;134:919. [PMC free article] [PubMed] [Google Scholar]S4.324.
Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333:13017. [PubMed] [Google Scholar]S4.325.
Versmissen J, Oosterveer DM, Yazdanpanah M, et al. Efficacy of statins in familial hypercholesterolaemia: a long term cohort study. BMJ. 2008;337:a2423. [PMC free article] [PubMed] [Google Scholar]S4.326.
Mortensen MB, Fuster V, Muntendam P, et al. A simple disease-guided approach to personalize ACC/AHA-recommended statin allocation in elderly people: the BioImage Study. J Am Coll Cardiol. 2016;68:88191. [PubMed] [Google Scholar]S4.327.
Willeit P, Kiechl S, Kronenberg F, et al. Discrimination and net reclassification of cardiovascular risk with lipoprotein(a): prospective 15-year outcomes in the Bruneck Study. J Am Coll Cardiol. 2014;64:85160. [PubMed] [Google Scholar]S4.328.
Nasir K, Bittencourt MS, Blaha MJ, et al. Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association cholesterol management guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2015;66:165768. [PubMed] [Google Scholar]S4.329.
Ridker PM, Mora S, Rose L, et al. Percent reduction in LDL cholesterol following high-intensity statin therapy: potential implications for guidelines and for the prescription of emerging lipid-lowering agents. Eur Heart J. 2016;37:13739. [PMC free article] [PubMed] [Google Scholar]S4.330.
Yano Y, ODonnell CJ, Kuller L, et al. Association of coronary artery calcium score vs age with cardiovascular risk in older adults: an analysis of pooled population-based studies. JAMA Cardiol. 2017;2:98694. [PMC free article] [PubMed] [Google Scholar]S4.331.
Malik S, Zhao Y, Budoff M, et al. Coronary artery calcium score for long-term risk classification in individuals with type 2 diabetes and metabolic syndrome from the Multi-Ethnic Study of Atherosclerosis. JAMA Cardiol. 2017;2:133240. [PMC free article] [PubMed] [Google Scholar]S4.332.
Sniderman AD, Tsimikas S, Fazio S. The severe hypercholesterolemia phenotype: clinical diagnosis, management, and emerging therapies. J Am Coll Cardiol. 2014;63:193547. [PubMed] [Google Scholar]S4.333.
Sniderman AD, Williams K, Contois JH, et al. A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk. Circ Cardiovasc Qual Outcomes. 2011;4:33745. [PubMed] [Google Scholar]S4.334.
Budoff MJ, Young R, Burke G, et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: the multi-ethnic study of atherosclerosis (MESA). Eur Heart J. 2018;39:24018. [PMC free article] [PubMed] [Google Scholar]S4.335.
Cholesterol Treatment Trialists (CTT) Collaborators, Mihaylova B, Emberson J, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:58190. [PMC free article] [PubMed] [Google Scholar]S4.336.
Huo X, Gao L, Guo L, et al. Risk of non-fatal cardiovascular diseases in early-onset versus late-onset type 2 diabetes in China: a cross-sectional study. Lancet Diabetes Endocrinol. 2016;4:11524. [PubMed] [Google Scholar]S4.337.
Svensson MK, Cederholm J, Eliasson B, et al. Albuminuria and renal function as predictors of cardiovascular events and mortality in a general population of patients with type 2 diabetes: a nationwide observational study from the Swedish National Diabetes Register. Diab Vasc Dis Res. 2013;10:5209. [PubMed] [Google Scholar]S4.338.
Guo VY, Cao B, Wu X, et al. Prospective association between diabetic retinopathy and cardiovascular diseasea systematic review and meta-analysis of cohort studies. J Stroke Cerebrovasc Dis. 2016;25:168895. [PubMed] [Google Scholar]S4.339.
Brownrigg JRW, de Lusignan S, McGovern A, et al. Peripheral neuropathy and the risk of cardiovascular events in type 2 diabetes mellitus. Heart. 2014;100:183743. [PubMed] [Google Scholar]S4.340.
Ogren M, Hedblad B, Engstrm G, et al. Prevalence and prognostic significance of asymptomatic peripheral arterial disease in 68-year-old men with diabetes. Results from the population study Men born in 1914 from Malm, Sweden. Eur J Vasc Endovasc Surg. 2005;29:1829. [PubMed] [Google Scholar]S4.341.
Pang X-H, Han J, Ye W-L, et al. Lower extremity peripheral arterial disease is an independent predictor of coronary heart disease and stroke risks in patients with type 2 diabetes mellitus in China. Int J Endocrinol. 2017;2017:9620513. [PMC free article] [PubMed] [Google Scholar]S4.342.
Waheed S, Pollack S, Roth M, et al. Collective impact of conventional cardiovascular risk factors and coronary calcium score on clinical outcomes with or without statin therapy: The St Francis Heart Study. Atherosclerosis. 2016;255:1939. [PubMed] [Google Scholar]4.4.High Blood Pressure or Hypertension
S4.41.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127248. [PubMed] [Google Scholar]S4.42.
Neter JE, Stam BE, Kok FJ, et al. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:87884. [PubMed] [Google Scholar]S4.43.
The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the Trials of Hypertension Prevention, Phase I. JAMA. 1992;267:121320. [PubMed] [Google Scholar]S4.44.
Whelton PK, Kumanyika SK, Cook NR, et al. Efficacy of nonpharmacologic interventions in adults with high-normal blood pressure: results from phase 1 of the Trials of Hypertension Prevention. Trials of Hypertension Prevention Collaborative Research Group. Am J Clin Nutr. 1997;65:652S660S. [PubMed] [Google Scholar]S4.45.
Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, phase II. The Trials of Hypertension Prevention Collaborative Research Group. Arch Intern Med. 1997;157:65767. [PubMed] [Google Scholar]S4.46.
Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:310. [PubMed] [Google Scholar]S4.47.
Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:111724. [PubMed] [Google Scholar]S4.48.
Appel LJ, Champagne CM, Harsha DW, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289:208393. [PubMed] [Google Scholar]S4.49.
Mozaffarian D, Fahimi S, Singh GM, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371:62434. [PubMed] [Google Scholar]S4.410.
He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325. [PubMed] [Google Scholar]S4.411.
Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA. 1998;279:83946. [PubMed] [Google Scholar]S4.412.
Aburto NJ, Ziolkovska A, Hooper L, et al. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013;346:f1326. [PMC free article] [PubMed] [Google Scholar]S4.413.
Graudal NA, Hubeck-Graudal T, Jrgens G. Effects of low-sodium diet vs. high-sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride (Cochrane Review). Am J Hypertens. 2012;25:115. [PubMed] [Google Scholar]S4.414.
Whelton PK, He J, Cutler JA, et al. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. JAMA. 1997;277:162432. [PubMed] [Google Scholar]S4.415.
Aburto NJ, Hanson S, Gutierrez H, et al. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013;346:f1378. [PMC free article] [PubMed] [Google Scholar]S4.416.
Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomised trials. J Hum Hypertens. 2003;17:47180. [PubMed] [Google Scholar]S4.417.
World Health Association. Guideline: Potassium Intake for Adults and Children. Geneva, Switzerland: World Health Organization, Department of Nutrition for Health and Development; 2012. [Google Scholar]S4.418.
Whelton PK, He J. Health effects of sodium and potassium in humans. Curr Opin Lipidol. 2014;25:759. [PubMed] [Google Scholar]S4.419.
Cornelissen VA, Smart NA . Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2:e004473. [PMC free article] [PubMed] [Google Scholar]S4.420.
Whelton SP, Chin A, Xin X, et al. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493503. [PubMed] [Google Scholar]S4.421.
Carlson DJ, Dieberg G, Hess NC, et al. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89:32734. [PubMed] [Google Scholar]S4.422.
Garca-Hermoso A, Saavedra JM, Escalante Y. Effects of exercise on resting blood pressure in obese children: a meta-analysis of randomized controlled trials. Obes Rev. 2013;14:91928. [PubMed] [Google Scholar]S4.423.
Rossi AM, Moullec G, Lavoie KL, et al. The evolution of a Canadian Hypertension Education Program recommendation: the impact of resistance training on resting blood pressure in adults as an example. Can J Cardiol. 2013;29:6227. [PubMed] [Google Scholar]S4.424.
Roerecke M, Kaczorowski J, Tobe SW, et al. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e10820. [PMC free article] [PubMed] [Google Scholar]S4.425.
Xin X, He J, Frontini MG, et al. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2001;38:11127. [PubMed] [Google Scholar]S4.426.
Stewart SH, Latham PK, Miller PM, et al. Blood pressure reduction during treatment for alcohol dependence: results from the Combining Medications and Behavioral Interventions for Alcoholism (COMBINE) study. Addiction. 2008;103:16228. [PMC free article] [PubMed] [Google Scholar]S4.427.
Dickinson HO, Mason JM, Nicolson DJ, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:21533. [PubMed] [Google Scholar]S4.428.
Wallace P, Cutler S, Haines A. Randomised controlled trial of general practitioner intervention in patients with excessive alcohol consumption. BMJ. 1988;297:6638. [PMC free article] [PubMed] [Google Scholar]S4.429.
Lang T, Nicaud V, Darn B, et al. Improving hypertension control among excessive alcohol drinkers: a randomised controlled trial in France. The WALPA Group. J Epidemiol Community Health. 1995;49:6106. [PMC free article] [PubMed] [Google Scholar]S4.430.
Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. [PMC free article] [PubMed] [Google Scholar]S4.431.
Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:95767. [PubMed] [Google Scholar]S4.432.
Sundstrm J, Arima H, Jackson R, et al. Effects of blood pressure reduction in mild hypertension: a systematic review and meta-analysis. Ann Intern Med. 2015;162:18491. [PubMed] [Google Scholar]S4.433.
Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387:43543. [PubMed] [Google Scholar]S4.434.
SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:210316. [PMC free article] [PubMed] [Google Scholar]S4.435.
Czernichow S, Zanchetti A, Turnbull F, et al. The effects of blood pressure reduction and of different blood pressure-lowering regimens on major cardiovascular events according to baseline blood pressure: meta-analysis of randomized trials. J Hypertens. 2011;29:416. [PubMed] [Google Scholar]S4.436.
Blood Pressure Lowering Treatment Trialists Collaboration. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384:5918. [PubMed] [Google Scholar]S4.437.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 2. Effects at different baseline and achieved blood pressure levelsoverview and meta-analyses of randomized trials. J Hypertens. 2014;32:2296304. [PubMed] [Google Scholar]S4.438.
Thompson AM, Hu T, Eshelbrenner CL, et al. Antihypertensive treatment and secondary prevention of cardiovascular disease events among persons without hypertension: a meta-analysis. JAMA. 2011;305:91322. [PMC free article] [PubMed] [Google Scholar]S4.439.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 7. Effects of more vs. less intensive blood pressure lowering and different achieved blood pressure levelsupdated overview and meta-analyses of randomized trials. J Hypertens. 2016;34:61322. [PubMed] [Google Scholar]S4.440.
Verdecchia P, Angeli F, Gentile G, et al. More versus less intensive blood pressure-lowering strategy: cumulative evidence and trial sequential analysis. Hypertension. 2016;68:64253. [PubMed] [Google Scholar]S4.441.
Bangalore S, Toklu B, Gianos E, et al. Optimal systolic blood pressure target after SPRINT: insights from a network meta-analysis of randomized trials. Am J Med. 2017;130:70719.e8. [PubMed] [Google Scholar]S4.442.
Bundy JD, Li C, Stuchlik P, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol. 2017;2:77581. [PMC free article] [PubMed] [Google Scholar]S4.443.
Ruggenenti P, Perna A, Loriga G, et al. Blood-pressure control for renoprotection in patients with non-diabetic chronic renal disease (REIN-2): multicentre, randomised controlled trial. Lancet. 2005;365:93946. [PubMed] [Google Scholar]S4.444.
Wright JT Jr, Bakris G, Greene T, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA. 2002;288:242131. [PubMed] [Google Scholar]S4.445.
Upadhyay A, Earley A, Haynes SM, et al. Systematic review: blood pressure target in chronic kidney disease and proteinuria as an effect modifier. Ann Intern Med. 2011;154:5418. [PubMed] [Google Scholar]S4.446.
Jafar TH, Stark PC, Schmid CH, et al. Progression of chronic kidney disease: the role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition: a patient-level meta-analysis. Ann Intern Med. 2003;139:24452. [PubMed] [Google Scholar]S4.447.
Lv J, Ehteshami P, Sarnak MJ, et al. Effects of intensive blood pressure lowering on the progression of chronic kidney disease: a systematic review and meta-analysis. CMAJ. 2013;185:94957. [PMC free article] [PubMed] [Google Scholar]S4.448.
Klahr S, Levey AS, Beck GJ, et al. The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. Modification of Diet in Renal Disease Study Group. N Engl J Med. 1994;330:87784. [PubMed] [Google Scholar]S4.449.
Emdin CA, Rahimi K, Neal B, et al. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313:60315. [PubMed] [Google Scholar]S4.450.
Arguedas JA, Leiva V, Wright JM. Blood pressure targets for hypertension in people with diabetes mellitus. Cochrane Database Syst Rev. 2013;CD008277. [PubMed] [Google Scholar]S4.451.
Margolis KL, OConnor PJ, Morgan TM, et al. Outcomes of combined cardiovascular risk factor management strategies in type 2 diabetes: the ACCORD randomized trial. Diabetes Care. 2014;37:17218. [PMC free article] [PubMed] [Google Scholar]S4.452.
Bress AP, Bellows BK, King JB, et al. Cost-effectiveness of intensive versus standard blood-pressure control. N Engl J Med. 2017;377:74555. [PMC free article] [PubMed] [Google Scholar]S4.453.
Soliman EZ, Byington RP, Bigger JT, et al. Effect of intensive blood pressure lowering on left ventricular hypertrophy in patients with diabetes mellitus: Action to Control Cardiovascular Risk in Diabetes blood pressure trial. Hypertension. 2015;66:11239. [PMC free article] [PubMed] [Google Scholar]S4.454.
ACCORD Study Group Cushman WC, Evans GW, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:157585. [PMC free article] [PubMed] [Google Scholar]S4.455.
Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:190313. [PubMed] [Google Scholar]S4.456.
Kassa B, Boissel J-P, Cucherat M, et al. Treatment of high blood pressure and gain in event-free life expectancy. Vasc Health Risk Manag. 2005;1:1639. [PMC free article] [PubMed] [Google Scholar]S4.457.
van Dieren S, Kengne AP, Chalmers J, et al. Effects of blood pressure lowering on cardiovascular outcomes in different cardiovascular risk groups among participants with type 2 diabetes. Diabetes Res Clin Pract. 2012;98:8390. [PubMed] [Google Scholar]S4.458.
Montgomery AA, Fahey T, Ben-Shlomo Y, et al. The influence of absolute cardiovascular risk, patient utilities, and costs on the decision to treat hypertension: a Markov decision analysis. J Hypertens. 2003;21:17539. [PubMed] [Google Scholar]S4.459.
Lonn EM, Bosch J, Lpez-Jaramillo P, et al. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374:200920. [PubMed] [Google Scholar]S4.460.
Neaton JD, Grimm RH Jr, Prineas RJ, et al. Treatment of Mild Hypertension Study. Final results. Treatment of Mild Hypertension Study Research Group. JAMA. 1993;270:71324. [PubMed] [Google Scholar]S4.461.
Julius S, Nesbitt SD, Egan BM, et al. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med. 2006;354:168597. [PubMed] [Google Scholar]S4.462.
Lawes CMM, Bennett DA, Lewington S, et al. Blood pressure and coronary heart disease: a review of the evidence. Semin Vasc Med. 2002;2:35568. [PubMed] [Google Scholar]S4.463.
Inder JD, Carlson DJ, Dieberg G, et al. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. 2016;39:8894. [PubMed] [Google Scholar]4.5.Tobacco Use
S4.51.
Carson KV, Verbiest MEA, Crone MR, et al. Training health professionals in smoking cessation. Cochrane Database Syst Rev. 2012;CD000214. [PMC free article] [PubMed] [Google Scholar]S4.52.
Patnode CD, Henderson JT, Thompson JH, et al. Behavioral counseling and pharmacotherapy interventions for tobacco cessation in adults, including pregnant women: a review of reviews for the U.S. Preventive Services Task Force. Ann Intern Med. 2015;163:60821. [PubMed] [Google Scholar]S4.53.
Stead LF, Koilpillai P, Fanshawe TR1, et al. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database Syst Rev. 2016;3:CD008286. [PMC free article] [PubMed] [Google Scholar]S4.54.
Pan A, Wang Y, Talaei M, et al. Relation of smoking with total mortality and cardiovascular events among patients with diabetes mellitus: a meta-analysis and systematic review. Circulation. 2015;132:1795804. [PMC free article] [PubMed] [Google Scholar]S4.55.
Mons U, Mezzinler A, Gellert C, et al. Impact of smoking and smoking cessation on cardiovascular events and mortality among older adults: meta-analysis of individual participant data from prospective cohort studies of the CHANCES consortium. BMJ. 2015;350:h1551. [PMC free article] [PubMed] [Google Scholar]S4.56.
Lv X, Sun J, Bi Y, et al. Risk of all-cause mortality and cardiovascular disease associated with secondhand smoke exposure: a systematic review and meta-analysis. Int J Cardiol. 2015;199:10615. [PubMed] [Google Scholar]S4.57.
Barua RS, Rigotti NA, Benowitz NL, et al. 2018 ACC Expert Consensus Decision Pathway on Tobacco Cessation Treatment: A Report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2018;72:333265. [PubMed] [Google Scholar]S4.58.
Anthenelli RM, Benowitz NL, West R, et al. Neuropsychiatric safety and efficacy of varenicline, bupropion, and nicotine patch in smokers with and without psychiatric disorders (EAGLES): a double-blind, randomised, placebo-controlled clinical trial. Lancet. 2016;387:250720. [PubMed] [Google Scholar]S4.510.
University of Southern California. Rx for change: clinician-assisted tobacco cessation. Available at: http://rxforchange.ucsf.edu/. Accessed January 30, 2019.4.6.Aspirin Use
S4.61.
Guirguis-Blake JM, Evans CV, Senger CA, et al. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2016;164:80413. [PubMed] [Google Scholar]S4.62.
Whitlock EP, Burda BU, Williams SB, et al. Bleeding risks with aspirin use for primary prevention in adults: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2016;164:82635. [PubMed] [Google Scholar]S4.63.
Lotrionte M, Biasucci LM, Peruzzi M, et al. Which aspirin dose and preparation is best for the long-term prevention of cardiovascular disease and cancer? Evidence from a systematic review and network meta-analysis. Prog Cardiovasc Dis. 2016;58:495504. [PubMed] [Google Scholar]S4.64.
Raju N, Sobieraj-Teague M, Bosch J, et al. Updated meta-analysis of aspirin in primary prevention of cardiovascular disease. Am J Med. 2016;129:e356. [PubMed] [Google Scholar]S4.65.
Ogawa H, Nakayama M, Morimoto T, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA. 2008;300:213441. [PubMed] [Google Scholar]S4.66.
Belch J, MacCuish A, Campbell I, et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ. 2008;337:a1840. [PMC free article] [PubMed] [Google Scholar]S4.67.
Fowkes FGR, Price JF, Stewart MCW, et al. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA. 2010;303:8418. [PubMed] [Google Scholar]S4.68.
Ikeda Y, Shimada K, Teramoto T, et al. Low-dose aspirin for primary prevention of cardiovascular events in Japanese patients 60 years or older with atherosclerotic risk factors: a randomized clinical trial. JAMA. 2014;312:251020. [PubMed] [Google Scholar]S4.69.
McNeil JJ, Wolfe R, Woods RL, et al. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med. 2018;379:150918. [PMC free article] [PubMed] [Google Scholar]S4.610.
Garca Rodrguez LA, Martn-Prez M, Hennekens CH, et al. Bleeding risk with long-term low-dose aspirin: a systematic review of observational studies. PLoS ONE. 2016;11:e0160046. [PMC free article] [PubMed] [Google Scholar]5.Cost and Value Considerations
S51.
Weintraub WS, Daniels SR, Burke LE, et al. Value of primordial and primary prevention for cardiovascular disease: a policy statement from the American Heart Association. Circulation. 2011;124:96790. [PubMed] [Google Scholar]S52.
Anderson JL, Heidenreich PA, Barnett PG, et al. ACC/AHA statement on cost/value methodology in clinical practice guidelines and performance measures: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:230422. [PubMed] [Google Scholar]S53.
Bress AP, Bellows BK, King JB, et al. Cost-effectiveness of intensive versus standard blood-pressure control. N Engl J Med. 2017;377:74555. [PMC free article] [PubMed] [Google Scholar]S54.
Moran AE, Odden MC, Thanataveerat A, et al. Cost-effectiveness of hypertension therapy according to 2014 guidelines. N Engl J Med. 2015;372:44755. [PMC free article] [PubMed] [Google Scholar]S55.
Park C, Wang G, Durthaler JM, et al. Cost-effectiveness analyses of antihypertensive medicines: a systematic review. Am J Prev Med. 2017;53:S13142. [PMC free article] [PubMed] [Google Scholar]S56.
Richman IB, Fairley M, Jrgensen ME, et al. Cost-effectiveness of intensive blood pressure management. JAMA Cardiol. 2016;1:8729. [PMC free article] [PubMed] [Google Scholar]S57.
Heller DJ, Coxson PG, Penko J, et al. Evaluating the impact and cost-effectiveness of statin use guidelines for primary prevention of coronary heart disease and stroke. Circulation. 2017;136:108798. [PMC free article] [PubMed] [Google Scholar]S58.
Odden MC, Pletcher MJ, Coxson PG, et al. Cost-effectiveness and population impact of statins for primary prevention in adults aged 75 years or older in the United States. Ann Intern Med. 2015;162:53341. [PMC free article] [PubMed] [Google Scholar]S59.
Heart Protection Study Collaborative Group. Statin cost-effectiveness in the United States for people at different vascular risk levels. Circ Cardiovasc Qual Outcomes. 2009;2:6572. [PubMed] [Google Scholar]6.Conclusion
S61.
Lehr AL, Driver SL, Stone NJ. The ABCDs of lifestyle counseling. JAMA Cardiol. 2016;1:5056. [PubMed] [Google Scholar]