What are 10 causes of obesity
Obesity: causes, consequences, treatments, and challenges
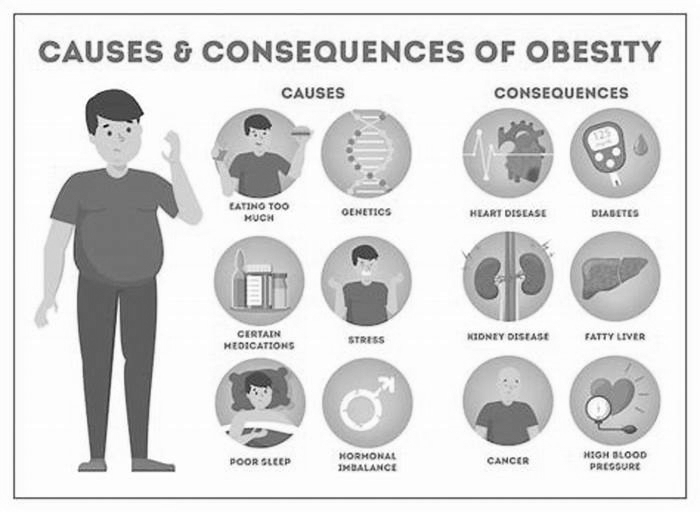
Obesity has become a global epidemic and is one of todays most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).
Obesity is mainly caused by imbalanced energy intake and expenditure due to a sedentary lifestyle coupled with overnutrition. Excess nutrients are stored in adipose tissue (AT) in the form of triglycerides, which will be utilized as nutrients by other tissues through lipolysis under nutrient deficit conditions. There are two major types of AT, white AT (WAT) and brown AT, the latter is a specialized form of fat depot that participates in non-shivering thermogenesis through lipid oxidation-mediated heat generation. While WAT has been historically considered merely an energy reservoir, this fat depot is now well known to function as an endocrine organ that produces and secretes various hormones, cytokines, and metabolites (termed as adipokines) to control systemic energy balance. Studies over the past decade also show that WAT, especially subcutaneous WAT, could undergo beiging remodeling in response to environmental or hormonal perturbation. In the first paper of this special issue, Cheong and Xu (2021) systematically review the recent progress on the factors, pathways, and mechanisms that regulate the intercellular and inter-organ crosstalks in the beiging of WAT. A critical but still not fully addressed issue in the adipose research field is the origin of the beige cells. Although beige adipocytes are known to have distinct cellular origins from brown and while adipocytes, it remains unclear on whether the cells are from pre-existing mature white adipocytes through a transdifferentiation process or from de novo differentiation of precursor cells. AT is a heterogeneous tissue composed of not only adipocytes but also nonadipocyte cell populations, including fibroblasts, as well as endothelial, blood, stromal, and adipocyte precursor cells (Ruan, 2020). The authors examined evidence to show that heterogeneity contributes to different browning capacities among fat depots and even within the same depot. The local microenvironment in WAT, which is dynamically and coordinately controlled by inputs from the heterogeneous cell types, plays a critical role in the beige adipogenesis process. The authors also examined key regulators of the AT microenvironment, including vascularization, the sympathetic nerve system, immune cells, peptide hormones, exosomes, and gut microbiota-derived metabolites. Given that increasing beige fat function enhances energy expenditure and consequently reduces body weight gain, identification and characterization of novel regulators and understanding their mechanisms of action in the beiging process has a therapeutic potential to combat obesity and its associated diseases. However, as noticed by the authors, most of the current pre-clinical research on beiging are done in rodent models, which may not represent the exact phenomenon in humans (Cheong and Xu, 2021). Thus, further investigations will be needed to translate the findings from bench to clinic.
While both socialenvironmental factors and genetic preposition have been recognized to play important roles in obesity epidemic, Gao et al. (2021) present evidence showing that epigenetic changes may be a key factor to explain interindividual differences in obesity. The authors examined data on the function of DNA methylation in regulating the expression of key genes involved in metabolism. They also summarize the roles of histone modifications as well as various RNAs such as microRNAs, long noncoding RNAs, and circular RNAs in regulating metabolic gene expression in metabolic organs in response to environmental cues. Lastly, the authors discuss the effect of lifestyle modification and therapeutic agents on epigenetic regulation of energy homeostasis. Understanding the mechanisms by which lifestyles such as diet and exercise modulate the expression and function of epigenetic factors in metabolism should be essential for developing novel strategies for the prevention and treatment of obesity and its associated metabolic diseases.
A major consequence of obesity is type 2 diabetes, a chronic disease that occurs when body cannot use and produce insulin effectively. Diabetes profoundly and adversely affects the vasculature, leading to various cardiovascular-related diseases such as atherosclerosis, arteriosclerotic, and microvascular diseases, which have been recognized as the most common causes of death in people with diabetes (Cho et al., 2018). Love et al. (2021) systematically review the roles and regulation of endothelial insulin resistance in diabetes complications, focusing mainly on vascular dysfunction. The authors review the vasoprotective functions and the mechanisms of action of endothelial insulin and insulin-like growth factor 1 signaling pathways. They also examined the contribution and impart of endothelial insulin resistance to diabetes complications from both biochemical and physiological perspectives and evaluated the beneficial roles of many of the medications currently used for T2D treatment in vascular management, including metformin, thiazolidinediones, glucagon-like receptor agonists, dipeptidyl peptidase-4 inhibitors, sodium-glucose cotransporter inhibitors, as well as exercise. The authors present evidence to suggest that sex differences and racial/ethnic disparities contribute significantly to vascular dysfunction in the setting of diabetes. Lastly, the authors raise a number of very important questions with regard to the role and connection of endothelial insulin resistance to metabolic dysfunction in other major metabolic organs/tissues and suggest several insightful directions in this area for future investigation.
Following on from the theme of obesity-induced metabolic dysfunction, Xia et al. (2021) review the latest progresses on the role of membrane-type I matrix metalloproteinase (MT1-MMP), a zinc-dependent endopeptidase that proteolytically cleaves extracellular matrix components and non-matrix proteins, in lipid metabolism. The authors examined data on the transcriptional and post-translational modification regulation of MT1-MMP gene expression and function. They also present evidence showing that the functions of MT1-MMP in lipid metabolism are cell specific as it may either promote or suppress inflammation and atherosclerosis depending on its presence in distinct cells. MT1-MMP appears to exert a complex role in obesity for that the molecule delays the progression of early obesity but exacerbates obesity at the advanced stage. Because inhibition of MT1-MMP can potentially lower the circulating low-density lipoprotein cholesterol levels and reduce the risk of cancer metastasis and atherosclerosis, the protein has been viewed as a very promising therapeutic target. However, challenges remain in developing MT1-MMP-based therapies due to the tissue-specific roles of MT1-MMP and the lack of specific inhibitors for this molecule. Further investigations are needed to address these questions and to develop MT1-MMP-based therapeutic interventions.
Lastly, Huang et al. (2021) present new findings on a critical role of puromycin-sensitive aminopeptidase (PSA), an integral non-transmembrane enzyme that catalyzes the cleavage of amino acids near the N-terminus of polypeptides, in NAFLD. NAFLD, ranging from simple nonalcoholic fatty liver to the more aggressive subtype nonalcoholic steatohepatitis, has now become the leading chronic liver disease worldwide (Loomba et al., 2021). At present, no effective drugs are available for NAFLD management in the clinic mainly due to the lack of a complete understanding of the mechanisms underlying the disease progress, reinforcing the urgent need to identify and validate novel targets and to elucidate their mechanisms of action in NAFLD development and pathogenesis. Huang et al. (2021) found that PSA expression levels were greatly reduced in the livers of obese mouse models and that the decreased PSA expression correlated with the progression of NAFLD in humans. They also found that PSA levels were negatively correlated with triglyceride accumulation in cultured hepatocytes and in the liver of ob/ob mice. Moreover, PSA suppresses steatosis by promoting lipogenesis and attenuating fatty acid -oxidation in hepatocytes and protects oxidative stress and lipid overload in the liver by activating the nuclear factor erythroid 2-related factor 2, the master regulator of antioxidant response. These studies identify PSA as a pivotal regulator of hepatic lipid metabolism and suggest that PSA may be a potential biomarker and therapeutic target for treating NAFLD.
In summary, papers in this issue review our current knowledge on the causes, consequences, and interventions of obesity and its associated diseases such as type 2 diabetes, NAFLD, and cardiovascular disease (Cheong and Xu, 2021; Gao et al., 2021; Love et al., 2021). Potential targets for the treatment of dyslipidemia and NAFLD are also discussed, as exemplified by MT1-MMP and PSA (Huang et al., 2021; Xia et al., 2021). It is noted that despite enormous effect, few pharmacological interventions are currently available in the clinic to effectively treat obesity. In addition, while enhancing energy expenditure by browning/beiging of WAT has been demonstrated as a promising alternative approach to alleviate obesity in rodent models, it remains to be determined on whether such WAT reprogramming is effective in combating obesity in humans (Cheong and Xu, 2021). Better understanding the mechanisms by which obesity induces various medical consequences and identification and characterization of novel anti-obesity secreted factors/soluble molecules would be helpful for developing effective therapeutic treatments for obesity and its associated medical complications.
10 Leading Causes of Weight Gain and Obesity
Obesity is one of the biggest health problems in the world.
Its associated with several related conditions, collectively known as metabolic syndrome. These include high blood pressure, elevated blood sugar and a poor blood lipid profile.
People with metabolic syndrome are at a much higher risk of heart disease and type 2 diabetes, compared to those whose weight is in a normal range.
Over the past decades, much research has focused on the causes of obesity and how it could be prevented or treated.
Many people seem to think that weight gain and obesity are caused by a lack of willpower.
Thats not entirely true. Although weight gain is largely a result of eating behavior and lifestyle, some people are at a disadvantage when it comes to controlling their eating habits.
The thing is, overeating is driven by various biological factors like genetics and hormones. Certain people are simply predisposed to gaining weight (
Of course, people can overcome their genetic disadvantages by changing their lifestyle and behavior. Lifestyle changes require willpower, dedication and perseverance.
Nevertheless, claims that behavior is purely a function of willpower is far too simplistic.
They dont take into account all the other factors that ultimately determine what people do and when they do it.
Here are 10 factors that are leading causes of weight gain, obesity and metabolic disease, many of which have nothing to do with willpower.
Obesity has a strong genetic component. Children of parents with obesity are much more likely to have obesity than children of lean parents.
That doesnt mean that obesity is completely predetermined. What you eat can have a major effect on which genes are expressed and which are not.
Non-industrialized societies rapidly develop obesity when they start eating a typical Western diet. Their genes didnt change, but the environment and the signals they sent to their genes did.
Put simply, genetic components do affect your susceptibility to gaining weight. Studies on identical twins demonstrate this very well (
Summary Some people appear to be genetically susceptible to weight gain and obesity.
Heavily processed foods are often little more than refined ingredients mixed with additives.
These products are designed to be cheap, last long on the shelf and taste so incredibly good that they are hard to resist.
By making foods as tasty as possible, food manufacturers are trying to increase sales. But they also promote overeating.
Most processed foods today dont resemble whole foods at all. These are highly engineered products, designed to get people hooked.
Summary Stores are filled with processed foods that are hard to resist. These products also promote overeating.
Many sugar-sweetened, high-fat junk foods stimulate the reward centers in your brain (3,
In fact, these foods are often compared to commonly abused drugs like alcohol, cocaine, nicotine and cannabis.
Junk foods can cause addiction in susceptible individuals. These people lose control over their eating behavior, similar to people struggling with alcohol addiction losing control over their drinking behavior.
Addiction is a complex issue that can be very difficult to overcome. When you become addicted to something, you lose your freedom of choice and the biochemistry in your brain starts calling the shots for you.
Summary Some people experience strong food cravings or addiction. This especially applies to sugar-sweetened, high-fat junk foods which stimulate the reward centers in the brain.
Junk food producers are very aggressive marketers.
Their tactics can get unethical at times and they sometimes try to market very unhealthy products as healthy foods.
These companies also make misleading claims. Whats worse, they target their marketing specifically towards children.
In todays world, children are developing obesity and becoming diabetic and addicted to junk foods long before theyre old enough to make informed decisions about these things.
Summary Food producers spend a lot of money marketing junk food, sometimes specifically targeting children, who dont have the knowledge and experience to realize they are being misled.
Insulin is a very important hormone that regulates energy storage, among other things.
One of its functions is to tell fat cells to store fat and to hold on to the fat they already carry.
The Western diet promotes insulin resistance in many overweight and individuals with obesity. This elevates insulin levels all over the body, causing energy to get stored in fat cells instead of being available for use (
While insulins role in obesity is controversial, several studies suggest that high insulin levels have a causal role in the development of obesity (
One of the best ways to lower your insulin is to cut back on simple or refined carbohydrates while increasing fiber intake (
This usually leads to an automatic reduction in calorie intake and effortless weight loss no calorie counting or portion control needed (
Summary High insulin levels and insulin resistance are linked to the development of obesity. To lower insulin levels, reduce your intake of refined carbs and eat more fiber.
Many pharmaceutical drugs can cause weight gain as a side effect (
For example, antidepressants have been linked to modest weight gain over time (
Other examples include diabetes medication and antipsychotics (
These drugs dont decrease your willpower. They alter the function of your body and brain, reducing metabolic rate or increasing appetite (
Summary Some medications may promote weight gain by reducing the number of calories burned or increasing appetite.
Leptin is another hormone that plays an important role in obesity.
It is produced by fat cells and its blood levels increase with higher fat mass. For this reason, leptin levels are especially high in people with obesity.
In healthy people, high leptin levels are linked to reduced appetite. When working properly, it should tell your brain how high your fat stores are.
The problem is that leptin isnt working as it should in many people who have obesity, because for some reason it cannot cross the blood-brain barrier (
This condition is called leptin resistance and is believed to be a leading factor in the pathogenesis of obesity.
Summary Leptin, an appetite-reducing hormone, doesnt work in many individuals who have obesity.
Another factor that dramatically influences peoples waistline is food availability, which has increased massively in the past few centuries.
Food, especially junk food, is everywhere now. Shops display tempting foods where they are most likely to gain your attention.
Another problem is that junk food is often cheaper than healthy, whole foods, especially in America.
Some people, especially in poorer neighborhoods, dont even have the option of purchasing real foods, like fresh fruit and vegetables.
Convenience stores in these areas only sell sodas, candy and processed, packaged junk foods.
How can it be a matter of choice if there is none?
Summary In some areas, finding fresh, whole foods may be difficult or expensive, leaving people no choice but to buy unhealthy junk foods.
Added sugar may be the single worst aspect of the modern diet.
Thats because sugar changes the hormones and biochemistry of your body when consumed in excess. This, in turn, contributes to weight gain.
Added sugar is half glucose, half fructose. People get glucose from a variety of foods, including starches, but the majority of fructose comes from added sugar.
Excess fructose intake may cause insulin resistance and elevated insulin levels. It also doesnt promote satiety in the same way glucose does (
For all these reasons, sugar contributes to increased energy storage and, ultimately, obesity.
Summary Scientists believe that excessive sugar intake may be one of the main causes of obesity.
People all over the world are being misinformed about health and nutrition.
There are many reasons for this, but the problem largely depends on where people get their information from.
Many websites, for example, spread inaccurate or even incorrect information about health and nutrition.
Some news outlets also oversimplify or misinterpret the results of scientific studies and the results are frequently taken out of context.
Other information may simply be outdated or based on theories that have never been fully proven.
Food companies also play a role. Some promote products, such as weight loss supplements, that do not work.
Weight loss strategies based on false information can hold back your progress. Its important to choose your sources well.
Summary Misinformation may contribute to weight gain in some people. It can also make weight loss more difficult.
If you have concerns about your waistline, you should not use this article as an excuse to give up.
While you cant fully control the way your body works, you can learn how to control your eating habits and change your lifestyle.
Unless there is some medical condition getting in your way, it is within your power to control your weight.
It often takes hard work and a drastic lifestyle change, but many people do succeed in the long run despite having the odds stacked against them.
The point of this article is to open peoples minds to the fact that something other than individual responsibility plays a role in the obesity epidemic.
The fact is that modern eating habits and food culture must be changed to be able to reverse this problem on a global scale.
The idea that it is all caused by a lack of willpower is exactly what food producers want you to believe, so they can continue their marketing in peace.