How to prevent disease in animals
Foot-and-Mouth Disease in Animals
The different virus serotypes of foot-and-mouth disease are not uniformly distributed within the endemic regions. Serotype O FMDV is responsible for approximately 70% of outbreaks globally. Six of the 7 serotypes have occurred in Africa (O, A, C, SAT-1, SAT-2, SAT-3), 4 in Asia (O, A, C, Asia-1), and 3 in South America (O, A, C). North and Central America, Australia, New Zealand, Greenland, Iceland, and Europe are now normally free of FMD (the last outbreak in Europe was in Bulgaria in 2011). There have been no reports of disease caused by serotype C FMDV anywhere since 2004, and it may now be eradicated outside of the laboratory. However, vaccination against this serotype still occurs in some places, so the complete absence of the virus in the field is difficult to prove.
The FMD virus is transmitted via direct contact with infected animals or indirect contact with secretions or excretions (including semen and milk) from infected animals or by mechanical vectors (people, horses, dogs, cats, birds, vehicles) or air movement over land or water. The virus can enter the host via inhalation, ingestion, or through skin wounds and mucous membranes. Breeding is a possible route of transmission for the SAT viruses in African buffalo populations.
A potential scenario for introduction of the virus into a previously FMD-free area is for a susceptible population, such as pigs, to be given imported food derived from an infected animal (meat or offal). Virus then spreads from pigs, which can expire up to 3,000 times more virus than cattle, to more susceptible cattle hosts via aerosol. Virus was reported to travel over water >250 km (~150 miles) from Brittany, France, to the Isle of Wight, UK, in 1981, but it usually travels no more than 10 km (~6 miles) over land. FMD has high agroterrorism potential because of its infectivity, high transmissibility through wind and by fomites, and the potential to cause enormous economic losses.
People can act as mechanical vectors of FMD by carrying virus on clothing or skin. However, FMD is not considered a public health problem.
FMD virus is environmentally resistant but can be easily inactivated outside the pH range 69 and by desiccation and at temperatures >56C. It is resistant to lipid solvents such as ether and chloroform, but sodium hydroxide (lye), sodium carbonate (soda ash), citric acid, and acetic acid (vinegar) are effective disinfectants. Iodophors, quaternary ammonium compounds, hypochlorite, and phenols are less effective disinfectants, especially in the presence of organic matter.
FMD virus is shed into milk in dairy cows before clinical signs develop, so there is opportunity for virus to spread from farm to farm and from cow to calf via raw milk. FMD virus may survive pasteurization depending on the method (high temperature short time, ultra high temperature, laboratory pasteurization); the lipid component of milk protects virus during heating. FMD virus can survive for up to 20 weeks on hay or straw bedding, in dry fecal matter for up to 14 days in summer, in fecal slurry for up to 6 months in winter, in urine for 39 days, and in soil for 3 (summer) to 28 (winter) days. However, the extent of virus survival in these materials is dependent on the initial level of contamination.
Vaccines against diseases transmitted from animals to humans: A one health paradigm
Three major epidemiological frameworks are identified for the control of zoonotic disease by means of vaccination of animals (). The scope of this review encompasses only those diseases for which a strategy targeting vaccination of animals is actually used or is under development. There are many diseases of animals transmissible to humans for which vaccination of animals is not feasible using currently available technologies, due to the complex ecology of the disease, a role of multiple wild animal species in transmission cycles, and difficulty of access to the host. For these diseases, the most practical and successful approach bypasses animals and is human immunization. Examples include yellow fever (acquired from mosquitoes infected by wild monkeys); hantavirus diseases (acquired by direct/indirect contact with rodents); and Ebola, Marburg, and severe respiratory coronavirus infections (acquired from contact with or aerosols generated by bats or from intermediate animal hosts infected by bats).
3.1. Framework I. Humans and domestic animals are dead-end hosts
The first major framework includes zoonotic infectious diseases that affect both humans and economically important animals, where wild animals are the source of infection. Livestock and humans are dead-end hosts, and neither contributes to the transmission cycle. In this case, vaccines are required to prevent disease in both humans and economically important animals, but do not interrupt transmission of the disease in nature. For Framework I diseases, there is an important opportunity to accelerate the development of new vaccines by concurrent veterinary and human product research (). Moreover the affected animal species represents a natural disease model of infection, pathogenesis and immunity that may be useful in testing efficacy and immunological correlates of protection of a new vaccine intended for human use, and thus provide data supporting regulatory approval under FDA's Animal Rule [9]. A list of Framework I diseases and vaccines is shown in , and an example is given below.
Table 2
Strengths and limitations of vaccination of animals as a means to control of zoonotic diseases.
| Framework (See ) | Strengths | Limitations |
|---|---|---|
| I | Benefits to human and animal health | DIVA requirements |
| Potential for accelerated development of new vaccines | Liability concerns | |
| Collaborations between animal and human health industry | Segregated regulatory pathways | |
| Reduced development costs | Inadvertent exposure of humans to live vaccines | |
| Additional models for Animal RuleLack of commercial incentive | ||
| II | New approaches to disease control | DIVA requirements |
| Benefits to human and animal health | Wild animal reservoirs | |
| Short development times and relatively low cost | Persistent environmental source of infection | |
| Accelerated regulatory pathway | Durability of immune response | |
| Potential for disease control without need for human vaccines | inadvertent exposure of humans to live vaccines | |
| Collaborations between animal and human health industry | Low commercial value, reliance on government funding | |
| Improved food safety | Feral animals or small farm operations inaccessible to vaccination | |
| High vaccine coverage required for herd immunity | ||
| III | New approaches to disease control | GMO issues |
| Control of infections acquired from wild animals | Safety for non-target species | |
| Accelerated regulatory pathway | Role of animals other than target species in transmission | |
| Potential for disease control without need for human vaccines | Very high or very low target species density | |
| Collaborations between animal and human health industry | Difficulty in designing and delivering oral vaccines | |
| Control of wildlife diseases | Vaccine stability under conditions of use | |
| Low commercial value, reliance on government funding |
3.1.1. West Nile virus disease
West Nile virus is a mosquito-borne, single strand, positive-sense, enveloped RNA virus (genus Flavivirus, family Flaviviridae), closely related to Japanese encephalitis virus. West Nile virus is a recognized cause of human disease ranging from mild fever-rash-headache syndromes to lethal encephalomyelitis. Horses, domesticated geese, farmed alligators (as well as a number of wild birds and mammals) are also susceptible to severe and fatal disease. Although recognized as a cause of disease as early as the 1940s, West Nile became an increasing problem in the 1990s, with outbreaks affecting humans and/or horses in northern Africa, Western Europe, the eastern Mediterranean, the Black Sea region and the Volgograd Oblast of Russia [10]. The most dramatic development was the introduction of West Nile virus into North America in 1999 [11], [12], [13], the occurrence of large outbreaks in 2002 and 2003, rapid spread across the US, and subsequent introduction to the Caribbean and South America. Horses and a number of wild bird species, notably crows and jays, were affected in addition to humans. Between 1999 and 2012, a total of 37,008 cases of West Nile fever and 16,196 cases of neuroinvasive West Nile disease were reported in the US, with the highest incidence in the middle of the country from Texas north to the Dakotas [14]. The incidence of neuroinvasive disease in the US has varied between 0.1 and 1.0 per 100,000 in this interval [15]. Over 25,000 horses have been affected since 1999, and in these animals the disease is more severe (33% case-fatality, 40% of survivors with neurological sequelae) than in humans (49% case fatality, 30% of encephalitis survivors with sequelae) [16]. Moreover, the incidence of West Nile in horses (700 per 100,000) is substantially higher than in humans [17].
The animal health industry rapidly responded to this veterinary emergency, and multiple West Nile vaccines were rapidly developed, including a live vaccine (discussed below), whole virion inactivated, DNA, and poxvirus vectored vaccines. The first vaccine for horses was marketed in 2001, only 2 years after introduction of the virus into the US. Multiple human vaccine development programs were also initiated, but many of these efforts were discontinued or decelerated due to the high market risk associated with low incidence, a slackening of public concern with the disease, and the uncertain regulatory pathway for vaccine approval. Although efficacy of a vaccine for equids is established [18], field trials to prove vaccine efficacy in humans would be large, expensive, and difficult due to the unpredictable occurrence of West Nile outbreaks. The application of the Animal Rule to licensing a West Nile vaccine, while plausible, has not been adjudicated by the FDA with a sponsor.
Although approaches to developing veterinary and human vaccines against West Nile were technologically similar, in only one case was a concurrent development program undertaken by a single company. This fact illustrates the current status of stove-piped and separate animal and human health biopharmaceutical industries. The exceptional case is of interest as a model of how vaccine development for zoonotic diseases could be improved. In 1999, within 2 months of the identification of West Nile as the etiological agent of the initial outbreak affecting humans and horses in New York, Acambis, a publically traded human-vaccine biotechnology company, applied its platform technology for yellow fever 17D-vectored vaccines to the development of a West Nile vaccine, with the intent to develop both vaccines for both horses and humans. This technology involved replacing the gene encoding the yellow fever 17D vaccine virus envelope (E) protein with the corresponding gene of West Nile virus. This chimeric vector vaccine platform had been previously used by the company to construct a chimeric vaccine against the closely-related Japanese encephalitis virus [19]; at the time, that vaccine had proven to be highly effective, protecting non-human primates against intracerebral challenge with virulent Japanese encephalitis virus [20]. Two new vectors were engineered, one with the wild-type West Nile NY99 strain E protein gene and one with an E gene containing three attenuating mutations [21], [22], [23]. The former was neurovirulent in mice, while the latter was more attenuated and thus deemed more suitable as a human vaccine. The principal question was whether the yellow fever 17D vector would infect and immunize horses, since yellow fever is a host-restricted primate virus. To find out, studies were sponsored by Acambis in early 2000 at the Colorado State University School of Veterinary Medicine. Horses were vaccinated with the West Nile/yellow fever chimeric virus or with yellow fever 17D vaccine, and viremia and antibody responses were determined [24]. In addition, vaccinated and control horses were challenged by the intrathecal injection of a high dose of virulent West Nile virus, following the same model referred to above for protection studies of the chimeric Japanese encephalitis vaccine wherein monkeys were challenged by the intracerebral route. These studies showed that horses inoculated with chimeric vaccine developed neutralizing antibodies against West Nile and were protected against a severe intrathecal challenge. A similar development plan was successfully followed for the mutated human vaccine version, using non-human primates as the test host. The veterinary and human vaccine candidates were developed side by side, and the data obtained in both programs were designed to support transition to advanced clinical trials in horses and humans. In 2002, Acambis licensed the veterinary vaccine technology to a major animal health company (Intervet), and in the same year clinical trial materials were made for human trials. Intervet completed development of the veterinary vaccine (PreveNile) [25], which was approved by USDA in 2007, and Acambis brought the human vaccine (ChimeriVax-WN02) into clinical trials in the same timeframe [26], subsequently outlicensing the technology to Sanofi Pasteur. As expected, development of the veterinary vaccine and its progression through the regulatory pathway substantially outpaced the human vaccine; importantly, the veterinary application significantly informed the human vaccine development program in providing useful information on safety, durability of immunity and immune correlates or protection.
Co-development of the veterinary and human West Nile vaccines is as a potential model for other vaccines. There are a few other examples where vaccines were co-developed for animals and humans, including vaccines against Venezuelan equine encephalitis and Rift Valley fever (described below). Certain issues arise, however, that may need to be considered in the context of such integrated efforts. First, a safety problem arising during use of a veterinary vaccine could provoke regulatory concerns or a liability problem for the human analog. Although a safety issue did arise briefly due to anaphylaxis type reactions in horses, resulting in temporary withdrawal of PreveNile from the market [27], there were no repercussions for the human analog vaccine (ChimeriVax-WN02). This raises the interesting question whether the human and veterinary regulatory agencies are integrating information that might be of value, either during development of similar vaccines for different species or after marketing approval. This is an obvious overlooked area for application of One Health principles. Second, the immune response to veterinary vaccines generally should differentiate naturally infected from vaccinated animals (DIVA) on the basis of a laboratory test, which allows compliance with trade restrictions. This is, of course not a concern for regulatory approval of human vaccines, although it can be useful in seroepidemiological and vaccine coverage studies. An example of problems associated with DIVA is the off-label use of commercial horse vaccine to protect emus against eastern equine encephalitis (EEE), since some combination vaccines against EEE contain equine influenza antigen and such vaccines elicit cross-reactive antibodies to avian influenza resulting in quarantine. The chimeric West Nile vaccine described above potentially allows for DIVA testing (using responses to the yellow fever nonstructural proteins expressed by the vector) [28].
3.2. Framework II. Domestic animals play a major role in transmission of the disease to humans (and domestic animals)
A number of important diseases are transmitted between domesticated animals and thence to humans. Vaccination of domesticated animals has the potential to protect humans against these zoonoses, either indirectly by interrupting transmission where domesticated animals are amplifying hosts in the transmission cycle or directly by preventing spread from infected animals to humans. A list of Framework II diseases and vaccines is shown in . Selected examples are used to illustrate the role of vaccination of domesticated animals in preventing human disease.
3.2.1. Brucellosis
Brucella spp. are facultative, intracellular Gram-negative bacteria, pathogenic for domestic animals and humans. Brucellosis, caused mainly by Brucella melitensis (which infects sheep and goats), Brucella abortus (cattle), and Brucella suis (swine), occurs worldwide, with the highest prevalence in the Middle East, Asia, Africa, tropical America, and the Mediterranean region [29], [30]. The annual incidence of human infections is estimated at 500,000 cases but the disease is widely acknowledged to be underreported [31]. Brucella canis, an infection of dogs, occurs worldwide with highest prevalence in tropical America. B. canis disease in humans has been reported, especially in persons handling breeding dogs and in immunosuppressed individuals. Human brucellosis is acquired by contact or aerosol spread from infected animals, fomites, or ingestion of unpasteurized milk or undercooked meat. Not surprisingly, Brucellae survive for long periods in dust, animal excreta, soil, meat and dairy products. Wild animals are also affected and can be the source of infection of livestock and humans. In animals, brucellosis causes epididymitis in males and abortion, placentitis, infertility and reduced milk production in female animals. The human disease is protean, manifested by chronic fatigue, relapsing fever, endocarditis, spondylitis, osteomyelitis, arthritis, and meningitis [32]. Prevention of human disease by control of brucellosis in livestock has long been a public health priority [33].
Control of brucellosis relies principally on surveillance, testing, removal of infected animals, import/export animal and animal product control provisions, protection from exposure to wild reservoirs (such as elk, deer, and bison), and vaccination. Antibiotic treatment of animals is regulated and discouraged due to the large doses and long treatment required and concern about resistance. Old, empirically developed live attenuated vaccines, B. melitensis rev1 vaccine for goats and sheep; B. abortus S19 and RB51 vaccines for cattle; and the oral B. suis S2 vaccine used widely in China for multiple species, elicit cellular immunity against the intracellular pathogen and are more effective than other types of vaccine [34]. The RB51 vaccine (a spontaneous rifampin-resistant rough mutant) is approved in the US [35]. However, the live vaccines have a number of drawbacks. The latter include lack of the ability to differentiate S1 and rev1 vaccine immunity from natural immunity (DIVA) and interference with surveillance and export control procedures; pathogenicity (especially abortion when animals are vaccinated during pregnancy); antibiotic resistance of the vaccine strains; and modest efficacy. Live vaccines used in livestock can also cause illness in humans. Vaccination as a stand-alone strategy has rarely been carefully evaluated, in large part due to concerns over the quality of the existing vaccines. However, vaccination is largely credited with elimination of brucellosis in the US [36], [37] (The US was declared free of brucellosis in cattle in 2009) and for control of brucellosis in China [38]. A recent study in Greece showed that a mass vaccination program with the B. melitensis rev1 vaccine resulted in a decrease in human infections [39]. A number of new vaccine approaches, including DIVA vaccines, designed to induce Th1 oriented cellular immunity are under investigation, including safer rationally designed, mutated live vaccines [34]; recombinant, invasive Escherischia coli[40]; recombinant subunit microencapsulated vaccines; and DNA vaccines [41]. Experimental B. canis vaccines have been investigated in mice.
Where brucellosis-free status has been achieved, as in the US, wild animal reservoirs (especially bison and elk) threaten to reintroduce the disease. Vaccination with existing vaccines is feasible, but delivery is challenging [42].
3.2.2. E. coli O157
This Vero cytotoxin secreting Gram-negative bacteria is an important cause of sporadic and epidemic food-borne illnesses of humans, including gastroenteritis and hemorrhagic colitis, with potentially lethal complications (hemolytic-uremic syndrome). Cattle and sheep are the principal reservoirs of infection and transmission to humans occurs via food (meat, seeds and vegetables) contaminated with animal feces. Undercooked ground beef is a source of infection in approximately one-third of human cases and recalls are a significant economic threat to the meat packing and distribution industry. Animals concentrated at feed lots and slaughter that shed bacteria can produce lots of meat with high rates of O157 [43], [44], but there is considerable variability in the occurrence of contaminations [45]. In developed countries, various sanitary measures and testing have been instituted to reduce the risk to consumers, but these remain imperfect. Vaccination of feed lot cattle has been proposed as a measure to reduce the prevalence and duration of shedding and the risk to consumers. O157-specific bacterial extract vaccines containing protective outer membrane proteins have been conditionally approved by USDA (manufactured by Epitopix, Willmar, MN) and fully approved by the Canadian Food Inspection Agency (Bioniche Life Sciences, Belleville, Ont.). Feedlot cattle receiving 2 or 3 doses of the Bioniche vaccine 34 weeks apart had 5998% reduction in colorectal colonization or fecal shedding and significant reduction in magnitude and duration of shedding [46], [47], [48].
Hurd and Malladi [49] modeled the impact of vaccinating cattle on human health outcomes. Assuming 80% efficacy of the vaccine and 100% adoption rate, the model indicated a 60% reduction in the incidence of E. coli O157-related human illness. The model also predicted significant reductions in the number of lots of contaminated ground beef and detection by USDA, which would have substantial economic benefit to packers and distributors. Vaccine effectiveness under conditions of field use will be highly dependent on adoption rate (vaccine coverage), and in part by whether cattle complete the 3-dose vaccination series on the proscribed schedule [46]. An interesting question is: who will pay for vaccination of feedlot cattle? Is the economic benefit there for the meat industry, and will vaccination reduce the cost of other preventive measures and testing or will vaccine costs simply be on top of other costs? Will government agencies concerned with human health subsidize the cost, without empirical demonstration of a human health benefit? Since ground beef only contributes about one-third of human infections, how could vaccines be used as a means of reducing other sources of food contamination? Another issue for use of the current vaccines is the role of other enterohemorrhagic E. coli (e.g. O26, O11, and O103) in human disease.
3.2.3. Cat scratch disease
This disease is caused primarily by the Gram-negative bacterium, Bartonella henselae, transmitted between domestic cats by the agency of cat fleas, Ctenocephalides felis. Human infection occurs by contact spread from cats, including scratches by claws contaminated with blood or flea feces, or possibly by flea bite [50], [51]. The prevalence of infection in household cats in the US is approximately 28%, but in stray animals it is 81% and high prevalence rates have been found in developing countries [52], [53]. Disease in humans is manifest by fever, a papule followed by a pustule at the site of infection and lymphadenopathy. Rare complications include meningitis, encephalitis, endocarditis, glomerulonephritis, osteomyelitis, neuropsychiatric abnormalities, and relapsing fever and splenomegaly. Human infections in immune-compromised individuals are particularly severe. Approximately 22,00024,000 cases and 2000 hospitalizations caused by cat scratch disease are estimated to occur annually in the US. In the late 1990s, Heska Corporation, an animal heath company in Colorado, initiated a program to develop a vaccine for household cats, with the goal of limiting the potential for transmission of the bacteria from cats to humans. Unfortunately, the program was not completed and no vaccine is available at present. Given the fact that cats rarely become ill with B. henselae, this would have been an unusual product providing protection to pet owners, with marginal if any real benefit to the target species. Moreover, it would likely have been extremely challenging to demonstrate a health benefit to humans.
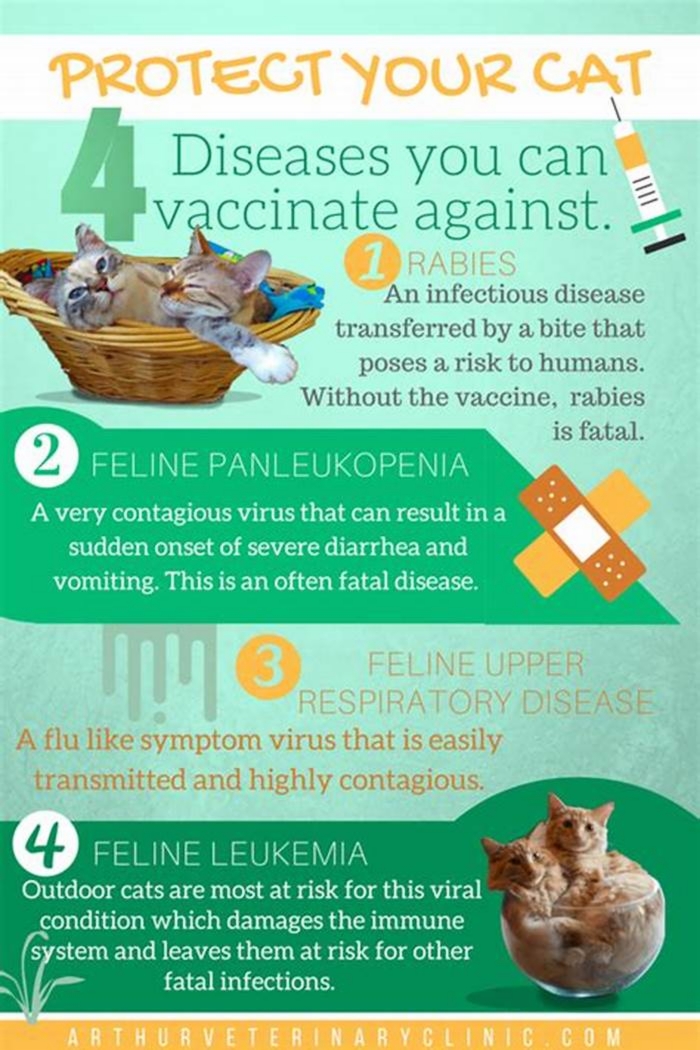
3.2.4. Rabies
Rabies is a fatal infection of the central nervous system caused by rabies virus, a member of the Lyssavirus genus, family Rhabdoviridae. It is estimated that up to 40,00060,000 cases of human rabies occur annually, and dog bite is the cause of over 98% [53]. Successful vaccination of dogs and humans against rabies was first demonstrated in 1885 by Louis Pasteur, using crude nerve tissue preparations. However, until the first decades of the 20th Century in developed countries, and continuing in many developing countries today, the ancient practice of dog population reduction campaigns have been the main approach to rabies control, a method that has repeatedly proven to be ineffective. Dog licensing and vaccination requirements were introduced in the United Kingdom in 1910, and gradually at the local and then state levels in the US beginning in the 1920s, with national requirements attained by 1955 [54]. Many successful dog vaccination campaigns have been reported in Latin American countries and Asia [55]. Some countries have declared eradication of canine rabies, notably the United Kingdom in 1922, Japan in 1956, the US in 2007, as well as Malaysia, Singapore, Taiwan, Hong Kong. In 2007, the first World Rabies Day event, the ultimate vision was promulgated of canine rabies elimination through systematic vaccination. However, rabies remains a significant public health problem, due to absent or incomplete dog vaccination in many areas of the world. More than 7.5 million post-exposure treatments with rabies vaccines are given annually, at a cost of over $1 billion worldwide [56], [57]. In China, due to the low prevalence of canine vaccination, the sales of rabies vaccines for human post-exposure prophylaxis outstrips any other human vaccine, accounting for 14% of all annual vaccine sales, i.e. 12 million doses costing $244 million [58]. The requirement for human post-exposure vaccination at this scale represents an obvious failure of public health, since it plays no role in containing the spread of rabies in the canine vector.
A very high rate of vaccine coverage in the dog population (exceeding 75%) is required for interruption of the rabies transmission cycle [59]. The development of oral rabies vaccines has allowed vaccination of free-roaming dogs that could not be restrained and vaccinated by injection, as well as the vaccination of wild animal species that are the source of infection in dogs [60]. Oral bait vaccine for dogs has been successfully deployed in trials in many countries, including Turkey, Thailand, Sri Lanka, South Africa, and the Philippines [61]; the World Health Organization has supported this approach as a supplemental program where there are substantial populations of free-ranging or feral dogs [60]. Significant increases in canine vaccination coverage have been achieved when oral rabies vaccine was added to a program of standard parenteral vaccination. Oral vaccination of dogs has been accomplished using commercial baits containing live modified rabies vaccines, such as the Street-Alabama-Dufferin (SAD) strain, variant B19 [62] and the attenuated Copenhagen strain of vaccinia expressing the rabies glycoprotein gene (G protein) [63].
A more detailed review of oral rabies vaccines is provided below (Framework III).
3.2.5. Hendra virus disease
Hendra virus disease, a severe and fatal infection of horses and humans in Australia, has been noted as an example illustrating One Health principles in disease prevention and control [64], and is especially relevant now that a new vaccine for horses has been introduced. Hendra is a member of the Henipavirus genus, family Paramyxoviridae. The reservoir hosts are fruit bats (Pteropus spp.), and the virus is spread from bats to horses by contact (including respiratory droplets), by food or fomites contaminated with bat urine, or by contact with sick horses. All reported human infections have resulted from contact with infected horses [65], [66], [67].
Hendra virus disease was first described in 1994. Human and equine cases have occurred in coastal Queensland and New South Wales and positive bats have been detected in the Northern Territory. A total of 81 deaths in equids have been reported in 14 outbreaks, with a very high case-fatality rate (75%), and 8 cases (4 fatal) have occurred in humans, including horse trainers and veterinarians, all of whom had contact with sick horses [68]. The disease is manifested by severe systemic illness, respiratory symptoms or acute and relapsing encephalitis [69]. Swine appear to be susceptible to experimental infection. Nipah virus, a closely related bat-borne agent in SE Asia has caused outbreaks of severe and fatal disease in swine and humans [65], [66], [67].
In November 2012, Pfizer Animal Health launched EquivacHeV, an adjuvanted subunit protein vaccine for the prevention of Hendra virus disease of horses in Australia [70]. Since horses are a major source of contact spread of Hendra virus to humans, the vaccine promises to make an important contribution to human health as well. Fear of acquiring the disease has also constrained equine veterinary practice in Australia [71], and the vaccine should mitigate this problem.
Development of EquivacHeV was a collaborative effort between Pfizer and CSIRO's Australian Animal Health Laboratory. However, support for the development program was also provided by human medical researchers in the US, at the Uniformed Services University of the Health Sciences supported by the Henry Jackson Foundation for the Advancement of Military Medicine. A provisional approval for limited use of the vaccine was obtained in early 2012, with full approval in November.
The vaccine is a soluble, recombinant glycoprotein (G) of Hendra virus, the ligand for cell attachment and antibodies to the protein neutralize cell receptor binding of the virus [72], [73]. The vaccine protects horses and ferrets against experimental infection [73], and appears to cross-protect against Nipah virus [74].
The availability of EquivacHeV should lead to rapid uptake by horse owners in Australia. The equine and horse racing industry in Australia is large, contributing billions of dollars, and over 1% of total Gross Domestic Product [75]. Hendra virus in horses is a notifiable disease in all Australian jurisdictions; the property where the horse cases are located is quarantined and animals that are infected are euthanized. The occurrence of at least one Hendra virus outbreak annually since 2006, and the high lethality of the disease have raised considerable awareness in Australia. Since all human cases of this zoonosis have resulted from contact with infected horses, vaccination of horses against Hendra virus promises to be a highly effective strategy for preventing human cases.
3.2.6. Rift Valley fever
Rift Valley fever is an enveloped, single-strand, segmented RNA virus belonging to the Phlebovirus genus, family Bunyaviridae, occurring in Africa, with intermittent extensions to the Arabian Peninsula. Rift Valley fever virus causes explosive and economically damaging outbreaks of disease in cattle and sheep, with stillbirth, abortion, and very high mortality of young animals; in adult animals, it causes 30% mortality in sheep, 1015% in cattle, and 510% in goats [76]. Humans typically develop self-limited nonspecific febrile illness, but 12% have a complicated course with hemorrhagic fever syndrome, encephalitis, hepatitis, renal failure, or retinitis, and case-fatality rates in severely ill and hospitalized patients is as high as 20% [77], [78]. The virus is transmitted between livestock and from livestock to humans by the agency of mosquito vectors. In addition, humans commonly acquire infection by contact and aerosol routes when handling, treating, or butchering infected livestock, and the virus can persist in meat for weeks. The ecology of Rift Valley fever and the reasons behind its periodic emergences have been the subject of intensive study. In brief, the reservoir of infection is Aedes mosquitoes, especially Ae. linneatopennis, which maintain the virus by transovarial transmission [79]. The dessication-resistant ova containing virus remain in depressions in the earth (dambos) that are flooded during the rainy season, with the subsequent emergence of infected adult Aedes mosquitoes. Infected, viremic, livestock in turn served as source for amplified virus transmission by a variety of mosquito vectors [76], [80].
There are no approved vaccines for prevention of Rift Valley fever in humans, although a number of candidates are in development by academic and government laboratories. Vaccination of cattle and sheep represents a strategy for preventing disease in these species, and thereby for interrupting virus transmission to humans. Rift Valley fever epizootics are to some extent predictable based on rainfall patterns and surveillance of disease in livestock [81]. Surveillance provides opportunities for rapid intervention, particularly with a single-dose vaccine (most likely a live, attenuated vaccine) that would protect against viremia in cattle and sheep and prevent mosquito infection. In addition, routine vaccination of livestock in inter-epizootic periods with a product capable of inducing durable protective immunity is a long range goal supported conceptually by modeling [82]. However, there are many obstacles to livestock immunization in Africa, including access, policy, regulatory approval, cold chain, and commercial viability. Additionally, DIVA requirements are driven by regulations prohibiting export of livestock or meat by countries experiencing Rift Valley fever [82].
Some of the obstacles to vaccination implementation could be overcome by development of improved vaccines. Two old veterinary vaccines, the live Smithburn vaccine, developed using techniques of serial passage in mouse brain similar to that applied to the early development of the French Neurotropic Vaccine against yellow fever [83], [84], and a formalin inactivated vaccine [85] are commercially available from the Onderstepoort Institute in South Africa. However, the Smithburn vaccine, now produced in BHK-21 cells, is reported to cause teratogenicity and abortion when used in pregnant animals [84] and is used only in countries endemic for Rift valley fever due to concerns about reversion. The inactivated vaccine, also grown in BHK-21 cell culture, requires multiple doses to be effective and probably has relatively short durability [86], making it less desirable for the interventions proposed above. Nonetheless, the inactivated vaccine was successfully used to interrupt a Rift valley fever outbreak in South African sheep [79]. Indeed, following a large epidemic of Rift Valley fever in Egypt in 197879, the Veterinary Serum and Vaccine Research Institute (Cairo, Egypt) produced a formalin-inactivated vaccine in BHK-21 cells using the epidemic strain (ZH501), which matched locally circulating strains compared to the South African strain [87]. Another inactivated vaccine (TSI-GSD 200) developed by the US Army for human immunization and grown in diploid fetal rhesus lung cells was tested clinically and shown to be well tolerated and immunogenic. Ninety % of the subjects developed a neutralizing titer >40, which was shown to be higher than the protective level in a passive immunization-challenge study in hamsters [88], [89]. In addition to the requirement for multiple doses for primary and booster immunization, inactivated Rift Valley fever vaccines have the disadvantage of requiring high biocontainment facilities for manufacturing.
In recent years, there has been substantial progress in development of newer vaccines, and some of these vaccine development projects have been collaborations between human and veterinary research groups. Additionally, there has been a moderate level of support from the US government because Rift Valley fever is a credible threat of natural or intentional (bioterrorist) introduction. Nevertheless, despite very promising technical results, there has been insufficient support from industry and government to propel any of these new vaccine candidates into use.
Because of the obvious advantages of rapid onset and durable immunity associated with live vaccines, development of an improved live vaccine has been the focus of research. US Army investigators attempted to induce attenuating mutations in two Rift Valley fever virus strains isolated during the 1978 Egyptian epidemic [90]. MP-12 is a live vaccine that was developed from the virulent ZH-548 strain by 12 passages in MRC-5 cells in the presence of the mutagen, 5-fluorouracil, resulting in a temperature sensitive virus with 9 amino acid mutations. Attenuation was demonstrated in multiple animal models, and reassortment studies showed that attenuating mutations were redundant and resided in all three gene segments [91], [92]. Development of MP-12 was undertaken by the US Army Medical Research Institute of Infectious Diseases with the intention to produce a vaccine for both human and animal immunization. The vaccine was clinically tested in 62 human volunteers and shown to be well-tolerated and highly immunogenic [93]. Army investigators, in collaboration with USDA, conducted a number of studies of MP-12 vaccine in sheep and cows, including neonatal, pregnant and lactating animals. These studies showed that MP-12 caused a low viremia, but with no attendant clinical signs; there was no virus secretion in milk, and no abortions or teratogenicity when vaccine was given in in mid- to late term pregnancy. MP-12 was highly immunogenic and protected livestock against virulent challenge [94], [95]. However, ewes vaccinated with MP-12 early in pregnancy showed a low incidence of abortion and teratogenicity, indicating some residual virulence of the vaccine [96]. To improve genetic stability and safety of MP-12, reverse genetic techniques were used to introduce deletions in the S and M RNA segments in genes encoding, respectively, NSs and NSm proteins [97], [98]. Two deletion mutants were evaluated for safety and immunogenicity in pregnant ewes [99] and in calves (Morrill JC personal communication, 2013) with positive results for the NSm deletant, making it an attractive candidate as a veterinary and human vaccine. There were no clear safety signals when ewes were inoculated in early-mid pregnancy. Further safety studies are required to rule out the low incidence of abortion/teratogenicity seen with parental MP-12 in early-term ewes. Unfortunately, human trials have not yet been performed with the rationally designed MP-12 derivative.
A third live vaccine designated Clone 13, is a plaque-derived clone of a Central African strain of Rift Valley fever isolated from a human subject, and was found to be naturally attenuated for mice and to have an in-frame deletion of most of the NSs gene [100]. This observation was the basis for modifying the MP-12 vaccine by NS gene deletion, as described above. Once again, a collaboration between the human and veterinary researchers led to a study in ewes, showing that Clone 13 was highly immunogenic but did not cause abortions [101], [102]. Another attenuated vaccine designated R566, has been developed by reassorting clone 13 and MP-12 so that it contains the S segment of clone 13 and the L and M segments of MP-12. This strain has attenuation domains from both parental vaccine candidates.
A number of live, replicating, and non-replicating heterologous viral vectors expressing Rift Valley fever G1 and G2 glycoproteins and nonstructural proteins have been have been investigated in mice, elicited immune responses and protected against challenge. The vectors included lumpy skin disease (capripoxvirus) [103], alphavirus (VEE and Sindbis) replicons [104], Newcastle disease virus [105], adenovirus, and Modified Vaccinia Ankara. Several of these constructs were used to immunize sheep and/or cattle (lumpy skin disease virus, Newcastle disease virus, and Sindbis replicons) with somewhat variable success. For a more comprehensive review see Indran and Ikegami [106] and Boshra et al. [107]. Live vectors are a promising approach for new Rift Valley fever vaccines, particularly veterinary vaccines, but may have problems for homologous boosting in light of anti-vector immunity. Various prime-boost strategies have been proposed, as for plasmid DNA vaccines (see below), but these would be exceptionally difficult to implement for immunization of livestock in the field, and are thus impractical.
Subunit protein produced in insect cells, virus-like particles [108], and DNA vaccines [109] against Rift Valley fever are also in early stage development. These approaches have potential advantages of safety and thermostability during storage and distribution, but may require multiple dosing and provide less durable immunity than live vaccines, and thus are less desirable products for Framework II implementation.
Overall, it remains to be seen which of the many Rift Valley fever vaccines in development progress to regulatory approval and whether an integrated veterinary and human health policy based on the immunization of livestock in Africa together with predictive surveillance, can abort impending outbreaks, and lead to long range control of this important disease.
3.2.7. Venezuelan equine encephalitis (VEE)
VEE is a mosquito-borne single strand, positive-sense, enveloped RNA virus belonging to the Alphavirus genus, family Togaviridae. Other medically important members of the Alphavirus genus include eastern and western equine encephalitis viruses. There are 6 VEE virus subtypes identified by antigenic and genomic analyses, and a number of additional varieties. Subtype IAB and IC cause epizootic disease in equids and associated zoonotic infections of humans [110]. During epizootics, horses and donkeys infected with these strains develop high viremias, serve as the primary hosts for infection of mosquito vectors and therefore are the indirect source of human infections acquired by mosquito bite. In contrast, the enzootic subtypes IIVI, are maintained in nature in cycles involving rodent species and mosquitoes, are not amplified by equid viremic hosts, and cause sporadic illness in humans and equid dead-end hosts. Epizootics of IC virus are the result of mutation and selection of virulent equine-competent viruses from enzootic strains, particularly the ID variant [111].
In the 19301940s VEE IAB viruses caused large epizootics in South America, with associated human epidemics of encephalitis. Between 1962 and 1969, a series of major subtype IAB and IC epizootics occurred in northern South America, and between 1969 and 1971 the virus spread north to Central America, Mexico, and Texas [112]. The cumulative economic and medical impact of VEE outbreaks between 1935 and 1971 was devastating, with over 150,000 equid and 50,000 human cases. Some of the VEE IAB epizootics are believed to have been spawned by the injection of horses with inactivated veterinary VEE vaccines containing residual live virus [113]. This likely occurred in Trinidad in 1943 and again in Nicaragua in 1970, but probably was a widespread problem in the past. Between 1992 and 1995, VEE IC re-emerged in Venezuela and Colombia, with an estimated 4000 equid deaths and over 100,000 human cases of which 3000 had encephalitis [114], [115].
Since VEE causes an acute incapacitating illness in humans and the virus efficiently infects via the aerosol route, it was developed by both the US and Soviet Union as an offensive biological weapon [116]. As part of these programs, vaccines for the protection of military personnel were also developed. In the US, a live, attenuated virus (TC-83) was developed by the US Army Medical Research & Development Command (USAMRDC) by empirical passages of the prototype Trinidad donkey (subtype IAB) virus in fetal guinea pig heart cell culture [117]. The development of the live vaccine followed poor experiences with chemically inactivated vaccines; in animal models, only the live vaccine protected against aerosol challenge. However, TC-83 vaccine has a number of drawbacks as a human vaccine, including failure to immunize about 18% of vaccinees, and moderate-to-severe reactogenicity in about 25% of subjects. In humans, it remains an investigational product, used solely for the protection of laboratory workers [118], with approximately 7000 persons vaccinated since 1963. The TC-83 virus acquired 12 mutations during the empirical passage series in guinea pig heart cells, but attenuation appears linked to only 2 of these, in the 5-noncoding region and the E2 envelope glycoprotein, and these substitutions appear to be subject to reversion in the vaccinated host [119]. In addition, TC-83 has been isolated from mosquito vectors during field use, illustrating the potential for secondary spread and mutation and recombination events. An investigational formalin-inactivated TC-83 vaccine (designated C-84) was also developed by USAMRDC and used following TC-83 priming to seroconvert TC-83 non-responders.
Since horses and related species are severely affected during epizootics and are the source of mosquito vectors infecting humans, there is an obvious need for a single dose veterinary vaccine that evokes rapid immunity. US Army investigators explored the use of TC-83 live, attenuated human vaccine for immunization of equids beginning in 1962 [120], and there was limited field use of the vaccine in Colombia in 1967. However, when epizootic VEE appeared for the first time in Central America (Guatemala) in May 1969, and then spread southwards to Costa Rica and northwards to the US, there was considerable urgency to utilize a vaccine strategy for control of the disease in horses, donkeys and mules. In 1969, the US military responded rapidly to requests for TC-83 vaccine from Guatemala and El Salvador. The vaccine had been produced and stockpiled at the Merrell National Laboratories, Swiftwater PA under contract to the USAMRDC for the purposes of biological defense. By 1972, over 10 million doses of TC-83 had been given to equidae in the US, Mexico and Central America [106]. Collaborative studies were also undertaken by agencies concerned with human and animal health (USAMRDC, NIH and USDA) to fully explore the biology of the vaccine in horses [121], [122], ultimately leading to licensure and commercialized by the animal health industry, both as a live vaccine and then an inactivated vaccine combo with eastern and western equine encephalitis vaccines. TC-83 vaccine was credited with a rapid curtailment of the 196971 outbreak. The history of VEE exemplifies many One Health principles, including the prevention of human cases through domesticated animal vaccination, use of a single vaccine product for animals and humans, and an agency (the US Army) concerned with human health engaged in both veterinary and human vaccine development, and providing a solution for curtailing an emerging zoonosis. After the large epizootic in the 1970s, TC-83 vaccine was again deployed during the epidemic in 1995 in Colombia to create an immune barrier to spread of the virus.
Recent efforts have focused on development of improved VEE vaccines for humans that are less reactogenic and more immunogenic than TC-83, can be manufactured in a more acceptable substrate, and have a lower risk of reversion to virulence and of mosquito transmission [123]. In addition, vaccines that cross-protect against the enzootic VEE subtypes are needed. VEE ID is endemic in Colombia, Peru, Venezuela, and Ecuador, and the IE subtype circulates in southern Mexico. Aguilar et al. [103] postulated that disease caused by VEE is confused clinically with dengue, and that, in endemic areas, up to 10% of dengue cases may actually be due to VEE enzootic subtype viruses. Subtype ID poses the ever-present risk of mutational change to produce high viremia and epizootic transmission in equids, as happened in the 1990s.
V3526 vaccine is a rationally designed vaccine from the epizootic Subtype IAB genome, with insertion of a PE2 cleavage-signal mutation combined with an E1 gene resuscitating mutation. V3526 had a good safety profile and was immunogenic and protective in laboratory animals, including nonhuman primates [124]. While retaining a degree of neurovirulence for suckling mice, V3526 is not virulent when inoculated intracranially in juvenile monkeys [125]. V3526 has also been evaluated in horses [126]. The vaccine was safe and highly immunogenic, with subcutaneous doses as low as 100 plaque-forming units shown to protect horses against challenge with virulent subtype IAB virus. Unfortunately, V3526 proved to be too reactogenic for humans in a Phase 1 trial [127], and thus development for both human and veterinary use has stopped. The V3526 virus was subsequently formalin inactivated and has been investigated with adjuvants replacement for the C-84 vaccine.
Other live and live vector approaches to improved VEE vaccines have been investigated only in laboratory animals, including a chimeric virus constructed from nonstructural genes of Sindbis and the structural genes from VEE [128], VEE replicon vaccines, and vaccinia recombinants. None of these approaches have reached advanced development.
It is only a matter of time before another VEE outbreak emerges in tropical America, and there is a substantial risk of cross-border spread. The prospects for vaccine interventions have diminished with dwindling support for new vaccines and increased concerns for vaccine safety.
3.3. Framework III. Wild animals play a major role in transmission of the disease to humans and domestic animals
Most zoonotic diseases are maintained in transmission cycles involving wild mammals or birds. However, because of the difficulties in vaccinating specific host species, wildlife immunization as a means of preventing spread to domestic animals and humans has been applied in only a few diseases. Some of the barriers to implementing wild animal vaccination include (i) involvement of multiple species in natural transmission cycles; (ii) safety concerns for non-target species; (iii) high reproductive rates and population turn-over; (iv) fastidious feeding behaviors and difficulty in designing effective baits; (v) difficult delivery due to very high or, conversely, very low population densities of the target species; (vi) environmental concerns, and release of genetically modified organisms; (vii) difficulty in designing an effective formulation for oral immunization; (viii) instability of a vaccine or vector under prevailing environmental conditions; and (ix) requirement for low unit cost and government funding for vaccine purchase and delivery. Nevertheless, targeted immunization of wild animal reservoirs is a subject of considerable interest for future research, not only for control of infectious agents affecting domestic animals and humans but also for control of wildlife diseases. One example of the latter was the effort to develop a means of immunizing great apes affected by Ebola virus in Central Africa with vaccines previously developed for human use.
Aside from rabies vaccines delivered in oral baits, which is well-established, wildlife vaccination has had limited success. Two promising examples of early-stage vaccine applications are described below (Lyme disease and Mycobacterium bovis). In addition experimental immunization and protection of prairie dogs (Cynomys ludovicianus) using a raccoon poxvirus recombinant oral bait vaccine [129], and ballistic vaccination of bison against B. abortus[130] have been described. Plague, a global but localized zoonotic disease with rodent wildlife reservoirs, would appear to be a target of particular interest for future research [131]. There are many other possible targets for new Framework III vaccines, and future research in this field is encouraged.
3.3.1. Lyme disease
In the United States, Lyme disease is the most common vector-borne disease and the 7th most common infectious disease overall. It is also a major and increasing public health problem in Europe. Approximately 30,000 cases are reported in the US annually, and the number has doubled in the last 15 years [132]. However, at a meeting in August, 2013, the Centers for Disease Control and Prevention (CDC) reported that the annual incidence of infection is believed to be 10-fold higher, i.e. 300,000 cases. Although Lyme disease occurs across the country, the incidence is highest in the northeast and north central states. In the US, Lyme disease is caused by the spirochete Borrelia burgdorferi, which is amplified each spring and summer in a cycle principally involving Ixodes scapularis ticks and field mice. Mice are persistently infected and represent the reservoir of infection in nature [133]. B. burgdorferi is passed transtadially to nymphal and adult ticks which infect humans and dogs; these species develop clinical disease but are dead-end hosts. The human disease is manifested by a protean syndrome, starting with a localized skin infection (erythema migrans), and progressing to a multisystem disease variably with lassitude, arthritis, carditis, meningitis and other neurological manifestations [134]. Because of the increasing incidence and geographic expansion of Lyme disease, the high incidence of tick exposure, and the difficulty in recognizing and removing attached ticks due to their small size, difficult differential diagnosis, troublesome and potentially severe clinical manifestations and medical controversies over treatment and chronicity of the disease, Lyme disease has emerged as a high priority for public health interventions [135].
Vaccination of humans would appear to be a logical and cost-effective means to prevent the disease [136], and veterinary vaccines for dogs are widely used and have proven to be modestly effective [137]. However, whereas safe and highly effective vaccines for humans have been developed, none is available for distribution today. Glaxo SmithKline's Lymerix vaccine was approved in 1998, but withdrawn in 2002 by the company, principally for commercial reasons, a decision that is lamentable given the increasing incidence of the disease [135], [138], [139]. A new Lyme disease vaccine for humans active against both B. burgdorferi and species causing Lyme disease in Europe developed by Baxter Bioscience is now in Phase II development, but it is uncertain whether it will reach the market. Nevertheless, these vaccines established critical immunological principles; the human vaccines are composed of recombinant OspA protein, the dog vaccines of both OspA and OspC, and work via antibody-mediated mechanisms. OspA is expressed by the Borrelia spirochete in the midgut of infected ticks. Since the tick vector only begins to transmit Borrelia 2436h after initiating blood feeding, OspA specific antibodies imbibed in the blood meal of a vaccinated host kill the bacteria and block transmission [140], [141].
If a similar OspA antibody response could be evoked in the natural reservoir hosts of B. burgdoferi (Peromyscus spp. field mice), it may be possible to interrupt the transmission cycle and reduce the prevalence of infected nymphal and adult ticks responsible for human and canine infections. Proof of concept was obtained in a field study where Peromyscus leucopus mice were trapped and vaccinated by subcutaneous injection of OspA; a reduction in the prevalence of B. burgdorferi in nymphal ticks was seen in the following year [142]. However, practical vaccine delivery and effective immunization of mice in the wild, requires a thermostable oral bait vaccine matched to the high population density and rapid population turnover of the reservoir hosts, the effects of which are not diluted by non-targeted species that play a role in B. burgdorferi transmission [135]. Two promising live oral vaccine approaches have been investigated in the laboratory: a bacterial (E. coli) vector [143], [144] and a viral vector (vaccinia) [145], [146] expressing OspA. The E. coli vector contained in an oral bait formulation and ingested multiple times elicited anti-OspA antibodies and protected laboratory and wild P. leucopus mice against needle and tick challenge. A 5-year field study of the oral bait vaccine, sponsored by CDC, has been performed and results are anticipated with interest. A company, US Biologics Inc., is engaged in bringing this vaccine to market. The vaccinia technology, which rests on the shoulders of the successful oral bait vaccine against wildlife rabies (see below), has been tested in the laboratory. Laboratory mice immunized by gavage with vaccinia expressing OspA were successfully immunized after a single dose and were protected against tick challenge. Peromyscus consuming oral bait vaccine were also significantly protected against challenge with infected ticks. Although the vaccinia vector looks promising, no commercial endeavor has yet emerged to support development. Both the E. coli and vaccinia oral vaccines require specialized formulations in baits that incorporate the vaccine in the bait itself, rather than in a liquid sachet embedded in the bait used for delivery of rabies vaccines.
Many questions surround the application of an oral bait vaccine targeting the reservoir host, including efficacy of this approach in the field, the high density of baits required, cost and sustainability of local and state funded programs aimed at distributing baits, and the role of species not targeted by the vaccine in Lyme disease maintenance cycles. If only partially effective, the risk of acquiring Lyme disease may be reduced, but the public would still need to take precautions against tick bite. Nevertheless, given the lack of a vaccine for humans, the high level of public concern about Lyme disease, the high risk to children, the localized nature of B. burgdorferi transmission allowing geospatially focused control efforts, and the possibility that homeowners may be motivated to play an active role in distributing baits, the idea has appeal.
3.3.2. M. bovis
M. bovis is the cause of tuberculosis in a wide array of domesticated and wild animals, and it remains a major veterinary health problem worldwide, causing severe economic losses from livestock disease, death and export restrictions. Humans become infected by ingesting raw milk or undercooked meat, or by the aerosol route from infected animals or humans. In developed countries where pasteurization and test-and-slaughter programs have controlled the disease, zoonotic infections are relatively rare, accounting for 0.37.2% of tuberculosis cases [147], [148], [149]; in developing countries which do not practice these measures, it remains more common, although few data on prevalence exist.
Wild animals are a major source of infection of domestic livestock [150]. Control measures aimed at control of M. bovis by culling wildlife reservoirs is problematic, with inconsistent results and ethical concerns. Vaccination of wildlife is an attractive alternative control measure, especially since the traditional tuberculosis vaccine (Bacille Calmette-Guerin, BCG) derived from M. bovis is effective when orally administered [151]. Examples of wildlife that serve as maintenance hosts of M. bovis and sources of infection in livestock, include white-tail deer in the US [152]; wild boar, red and fallow deer in Europe [153]; badgers in the United Kingdom [154]; African buffalo (Syncerus caffer) in South Africa [155]; and brushtail possums (Trichosurus vulpecula) in New Zealand [156].
Brushtail possums have been experimentally vaccinated using oral BCG and shown to be resistant to challenge with M. bovis[157]. Proof of concept has been provided by a field study in an endemic area of New Zealand. Possums were trapped, manually vaccinated using orally delivered BCG in a lipid matrix formulation, and vaccinated and control animals were recaptured at intervals [158]. Vaccinated animals received 13 vaccinations during the 2-year study. At the end of study, the 14ha study area was depopulated, and all animals assessed for clinical and subclinical M. bovis infections. Vaccine efficacy against naturally acquired tuberculosis was 9596%. The authors concluded that oral vaccination of possums could be a practical strategy contributing to elimination of M. bovis in livestock. Although the field study did not demonstrate control via freely consumed bait vaccine, captive possums have been shown to consume vaccine in flavored baits [159].
3.3.3. Rabies
Rabies is transmitted between specific wild carnivore reservoir hosts, which serve as a source of spill-over infections of other wild carnivores, and infection of domesticated animals and humans. Oral rabies vaccine was initially deployed in Europe for control of rabies in the red fox (Vulpes vulpes), using modified live virus vaccine [160], [161]. The concept began in the 1960s with the work of George Baer at the CDC, which showed that foxes could be orally immunized with modified live virus [162]. The live, attenuated Evelyn-Rokitnicki-Abelseth (ERA) vaccine or Street-Alabama-Dufferin (SAD) viruses were employed in experimental and field studies. Numerous studies in the 1970s confirmed that captive and wild foxes could be orally immunized with a variety of baits containing vaccine [163]. In 1978, Steck and colleagues initiated a wild fox rabies control program in the Swiss Alps using oral bait vaccine consisting of chicken heads with vaccine and tetracycline biomarker in a container made of polyvinyl chloride and aluminum foil inserted under the scalp [164]. The trial demonstrated that 60% of foxes had ingested bait. Over the next 20 years, successful fox rabies control programs were carried out in many European countries, after the late 1980s using baits distributed by fixed wing aircraft and helicopters rather than by ground [165], and resulting in elimination of terrestrial rabies in several countries [166], [167]. For large scale distribution, the laborious chicken head method bait gave way to commercially manufactured molded or extruded baits of various kinds, consisting of fish meal or bone meal, fat, and a pouch or blister containing liquid vaccine virus [168]. The vaccines currently used in Europe are (1) SAG2 (e.g., RABIGEN, Virbac Laboratories, France), a modified live attenuated rabies virus derived from the original SAD vaccine and having an additional mutation in the codon for amino acid 333 of the rabies G protein, which increases genetic stability of the virus [169]; and (2) recombinant vaccinia virus (Copenhagen strain) expressing the ERA strain rabies G protein (Raboral, Merial Corp.) [170]. The rabies G protein gene has been inserted into the thymidine kinase gene of vaccinia, which results in further attenuation compared to the parental virus [171], [172]. Duration of oral rabies immunity, at least 18 months in adult red foxes, is sufficient to provide herd immunity and reduce the reproductive rate (R0) to less than 1.
The modified live virus vaccines are more thermolabile than vaccinia, require 20C storage, retain some pathogenicity for non-target species, and pose safety risks to humans exposed inadvertently. Consequently, recombinant vaccinia is the only oral rabies vaccine approved for wildlife immunization in the US. This vaccine consists of fishmeal and fish oil bound by a polymer (ethylene vinyl acetate) and containing the vaccine in a plastic pouch held in place by a wax mixture.
Immunization with vaccinia or modified live virus occurs in the buccal mucosa and tonsils, and vaccines are poorly effective after ingestion [173]. In one study, consumption by red foxes of a single bait containing vaccinia resulted in protection against virulent rabies in only half of the animals [174]. This observation suggests that high bait densities and repeated vaccinations are important to effective control in the wild. Bait densities distributed in Europe generally range between 10 and 20 baits/km2, resulting in 5080% of animals potentially immunized (positive for the tetracycline biomarker) [161]. In addition to distribution density, feeding habits may also be important, since animals have been observed to pick apart baits and consume only the bait portion.
While control of terrestrial wildlife rabies has been successful in parts of Europe, it has been more challenging in other areas due to the diversity of carnivores involved in transmission of different rabies virus variants. In the arctic regions, a specific rabies variant is maintained in the arctic fox, with spill-over infections of red foxes, skunks, and raccoon dogs. Where vaccination is not practiced in domesticated sledge dogs, these animals may be severely impacted by contacts with rabid foxes, and human dog owners placed at considerable risk. While experimental oral vaccination of arctic foxes has been successful, there is limited experience in the field [175]. In Ontario, Canada control of arctic rabies variant in red foxes using oral bait vaccine has been successful, but the virus still occurs as a result of spill-over transmission to skunks, which are not efficiently immunized with recombinant vaccinia vaccine [176], [177].
Oral bait recombinant vaccinia vaccine has been primarily used to control raccoon rabies, which expanded beginning in the mid-1970s from enzootic areas in Florida northwards and westwards to involve many states in the eastern US, as well as New Brunswick and Quebec, Canada [178], [179]. The control program relies on distribution of vaccine baits specific zones of rabies activity, particularly along the Appalachian Ridge, enhanced surveillance and ring vaccination with evidence of spread of the disease. Judged from the absence of spread beyond the zones of vaccine distribution, the program has worked well, despite relatively low prevalence of rabies antibody (approximately 30%) in sampled raccoons [170]. It is possible that pre-existing immunity to raccoonpox virus may interfere with immunization with vaccinia [180]. The economics of large-scale oral vaccination programs in the US have been modeled and are generally favorable [181]. In addition to control of raccoon rabies, successful use of the vaccine has been made in the control of gray fox (Urocyon cinereoargenteus) variant rabies in west Texas [182]. In contrast to raccoons, a higher prevalence of rabies antibody (61%) attributed to vaccination is found in gray foxes. Rabies in coyotes (Canis latrans) was responsible for epizootic canine rabies in the 1980s and 1990s in parts of the US, and was controlled by an oral bait vaccination campaign, contributing to the elimination of canine rabies by 2007 [177].
Skunks remain a problematic species for vaccine control of rabies. Skunks are an important spill-over host for the arctic fox, raccoon rabies, and big brown bat rabies virus variants [183]. Although the vaccinia vector vaccine is not sufficiently effective in skunks [169], promising results were obtained with a replication-competent adenovirus type 5 vector expressing the rabies G protein [184]. Aerial distribution of this vaccine (ONRAB, Artemis Technologies, Guelph) showed high rates of immunization of raccoons, and arctic foxes and modest seroconversion (1751% in different plots) in skunks, probably due to lower rates of bait acceptance [185], [186]. ONRAB is approved by the Canadian regulatory authorities for control of rabies in skunks, raccoons, and foxes, and is under investigation in the US.